Author: Mitchell Webb
When our intelligent and necessary emotion – ANGER – becomes unhealthy and damagingWhen our intelligent and necessary emotion – ANGER – becomes unhealthy and damaging
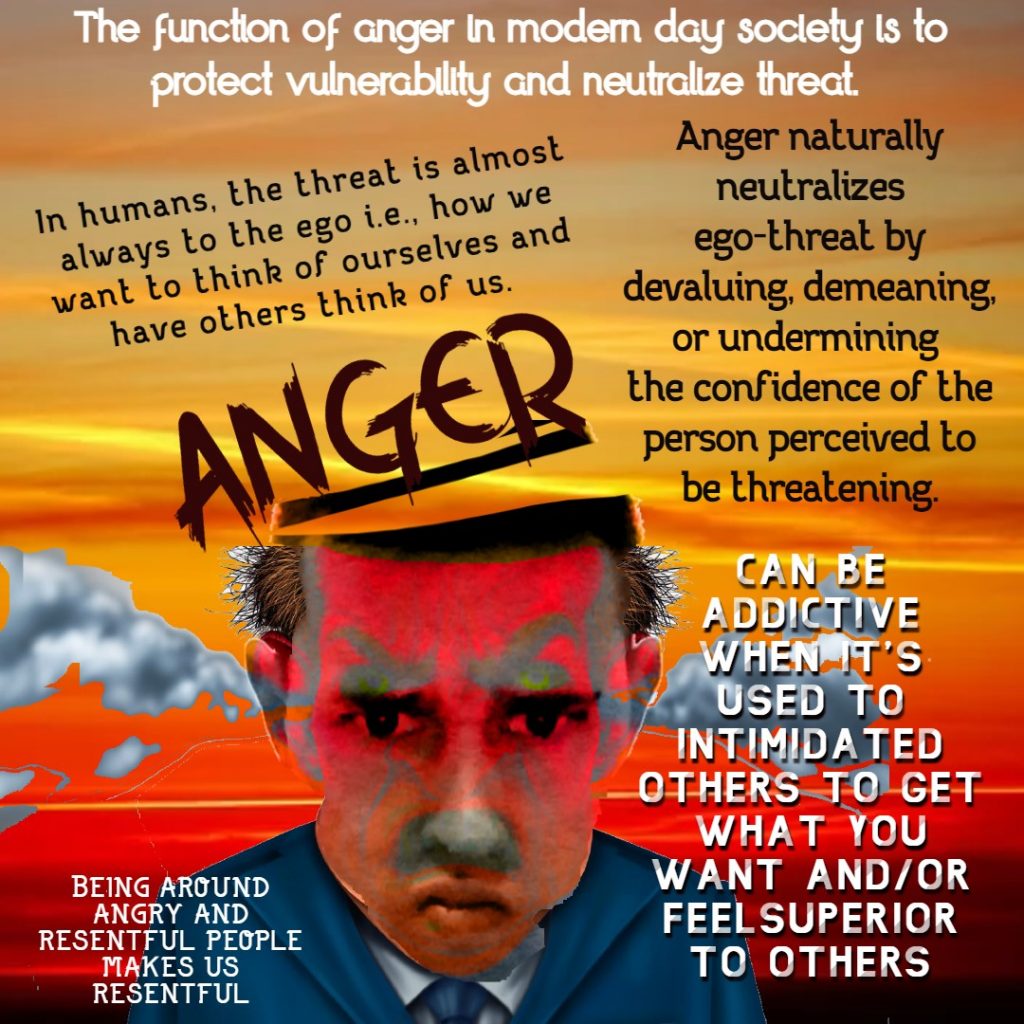
The function of anger is to protect vulnerability and neutralize threat.
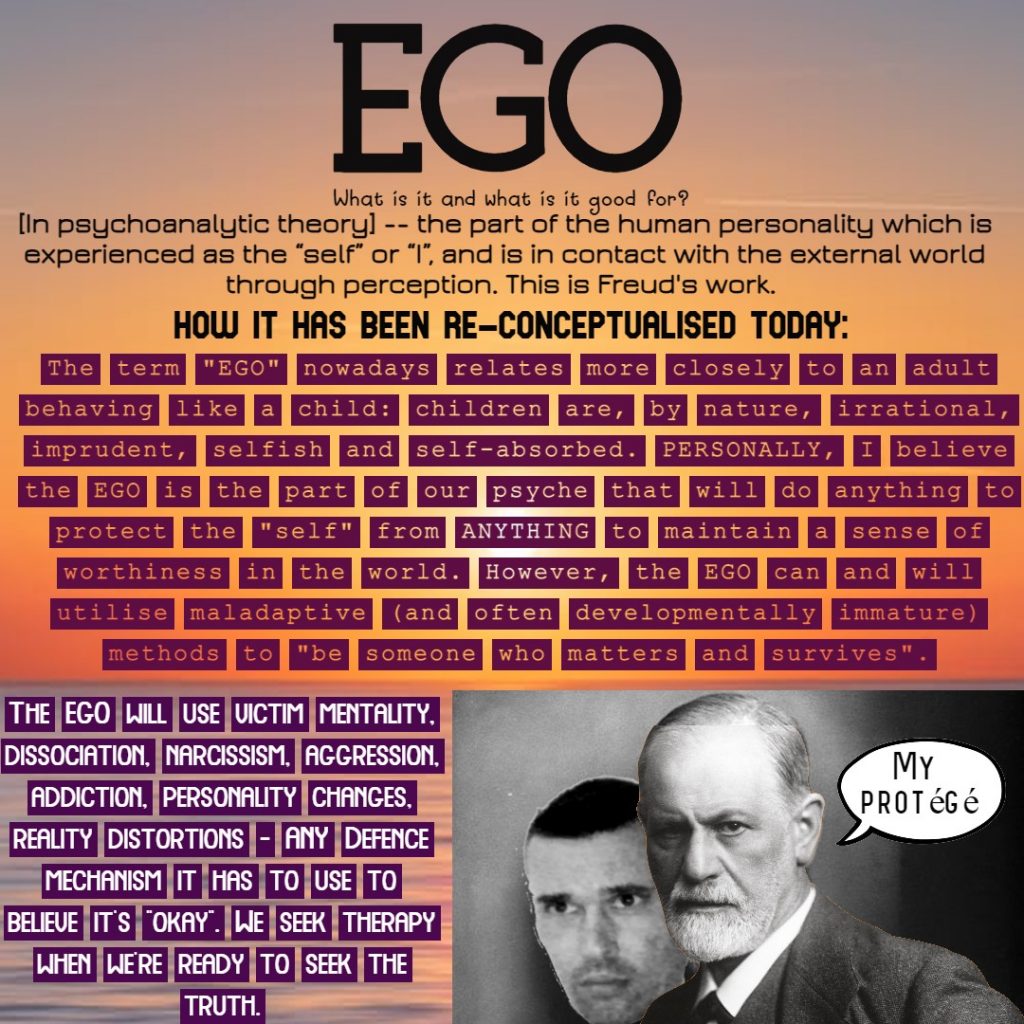
The threat humans cognitively perceive is almost always to the ego i.e., how we want to think of ourselves and have others think of us. Anger neutralizes ego-threat by devaluing, demeaning, or undermining the “power” of the person perceived to be threatening. Humans get angry when they don’t get what they want, when they’re disrespected, or when they perceive something is unjust/unfair. Anger, the emotion, is a chemical messenger. It communicates to us, to others, and motivates us to act, speak, do something. Healthy responses to anger include being assertive, feeling empowered, protecting ourselves and love ones from ACTUAL threat, setting boundaries with others, and making social change for justice (for example). It becomes unhealthy when we become passive-aggressive, violent, vengeful, spiteful, aggressive, resentful, sarcastic, “moody”, rude etc.
Receive the message and respond from a wise, calm place after the intensity of the emotion has past. Sometimes we have to act in the moment. Our ancestors may have required this for fight/flight survival. These days, we can generally PAUSE and calm the self before responding from a mindful and compassionate heart and mind. Remember: Hurt people, hurt people.
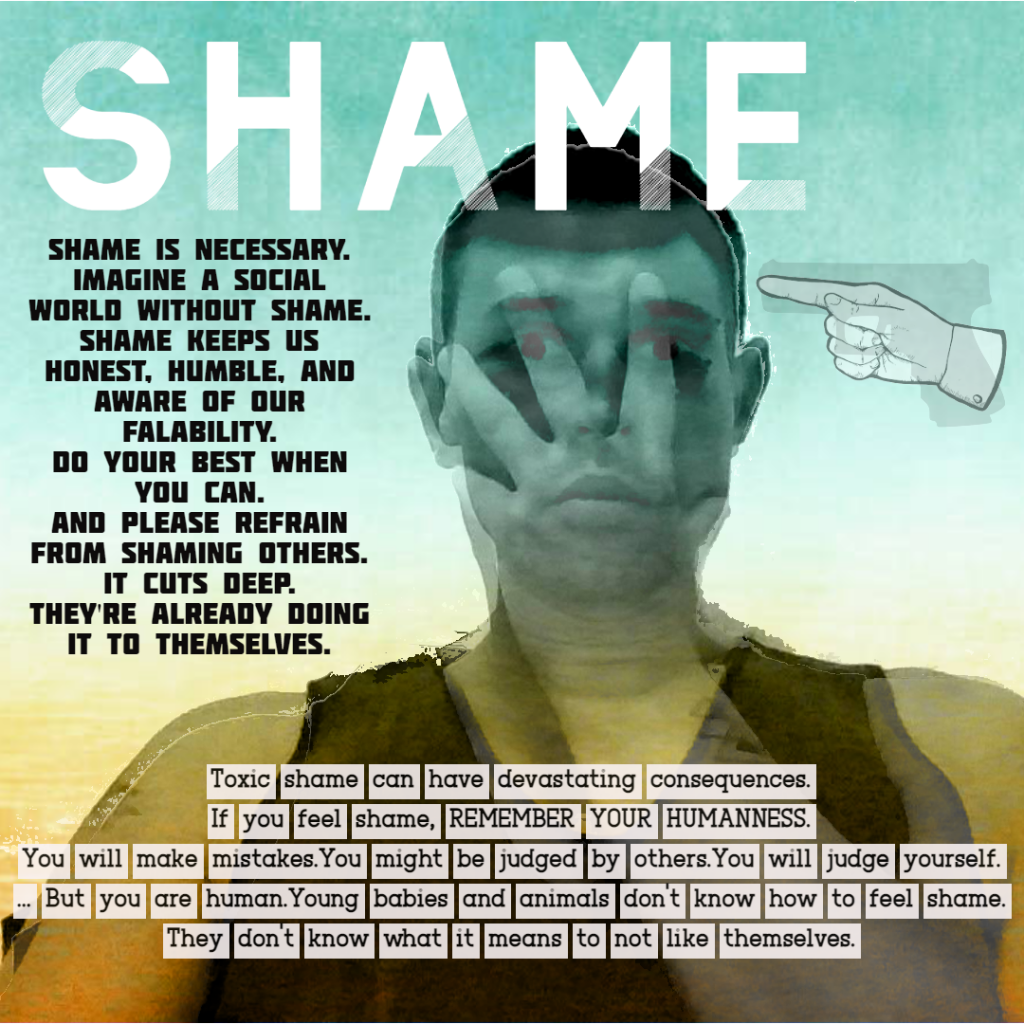
Toxic Shame and the Gifts of Healthy Shame.Toxic Shame and the Gifts of Healthy Shame.
Think about what it means to be human. Yes, we have internalised toxic levels of pressure to be a certain way. We also know, as we mature, that being a certain way it complete bull shit and nonsense. I saw a quote once that said “Can you remember who you were, before the world told you who you should be?” -Charles Bukowski. I don’t know who this person is, but it’s the truth. Come home to yourself, and reach out for help from a professional if you need some support or help with that.
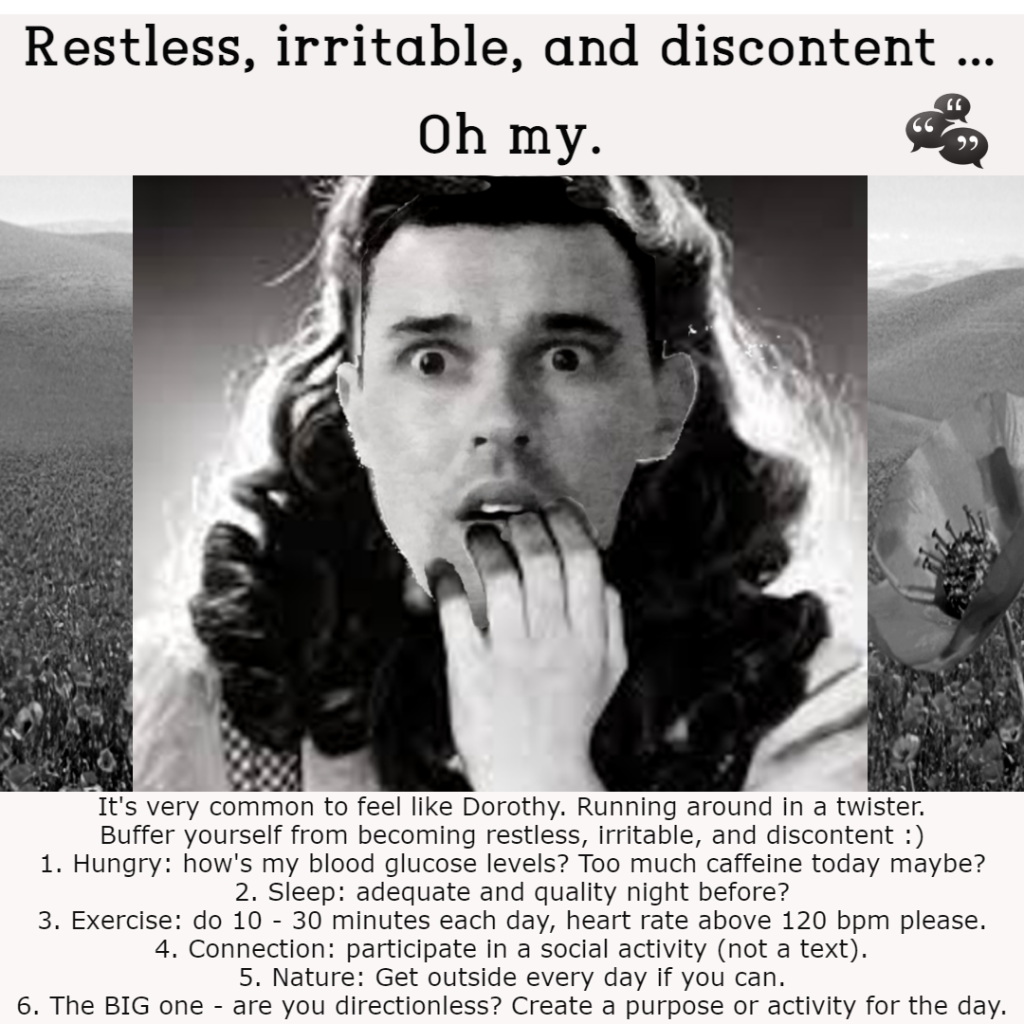
Are you feeling Restless, Irritable, and Discontent?Are you feeling Restless, Irritable, and Discontent?
I would infer that you may be depleted in some area of your life. Generally, when I am having any of these experiences I can recognise that my basic needs, and possibly even transformative, needs are not met. My basic needs are food and water, adequate sleep, shelter and safety, social connection (belonging), and esteem needs (e.g., self-respect, self-worth, self-competence, mastery and achievement, integrity, sense of freedom and independence etc.). Perhaps only when all my deficiency needs are met, and I’m experiencing dissatisfaction with my growth needs, do I feel Restless, Irritable, and Discontent in this area of my life – however I assume some would argue that if I am feeling that way when attending to my growth needs, then I may have slipped back to Esteem Needs. You can look up Maslow’s Hierarchy of Needs for a visual representation if you like, using a search engine. Below is a GIF that I created to educate people on how we can buffer ourselves to vulnerabilities. It’s very telling to go into the body when we haven’t eat for a while, may be we’re running on caffeine, and you can feel the restlessness in the body. We have to fuel up when we’re hungry to buffer ourselves from becoming irritable and restless. If you’re feeling discontent with life, I would suggest a social activity, play time with friends, working on a project of some kind, or getting involved in your community.
What is your intention? Why “will power” is often not enough.What is your intention? Why “will power” is often not enough.
Adapted from AIPC (2022), Institute Inbrief, Issue 363.
Oftentimes, a brand new year is used like a clean slate. We can do this any time throughout the year, however, I understand that there is an added element of our “collective consciousness” in the universal atmosphere motivating us with some renewed energy and will. At this time of year, humans perceive that everyone else is also feeling hopeful, invigorated, and full of promise. But the road to realisation of goals is littered with the carcasses of broken dreams, unfulfilled promises, and intentions that dissipated in the stress and mundane of everyday life – our goals did not receive the “oxygen” required to be sustainable.
What is our “Will”?
Have you ever fallen short of accomplishing you New Year’s Resolution? Sometimes, even before the end of New Year’s Day? People many think, “I don’t have the will power to sustain it”, however, if we look at this from the perspective of Psychosynthesis, a transpersonal psychology, we will understand why our understanding of “will power” if often incorrect. If you did anything today, you have will inside you. You have drive, motive, and energy.
While our will may not have all the “power” that we would like it to have, our will is always present with us, somewhere. Psychosynthesis counsellors, especially trained to be observant about will, acknowledge that one of their sacred duties with clients is to track their will, but all mental health professionals can tune more into the willing function of self, for the ultimate good of the client. What do we need to know to do that?
First, will isn’t just desire energy. It is not synonymous with control, it is not about “strong-arming” someone, and it isn’t merely about repressing undesirable material.
Personal and transpersonal will
At a personal level, “will” can be understood as an essential impulse toward our own wholeness. It is that drive within us which coordinates the often-conflicting parts of our personalities into self-expression. As the function closest to the self, it regulates and directs other functions, such as imagination, intuition, impulses, sensations, thoughts, and feelings. It is will which guides us toward personal integration. As we align our lives with a broader vision for what we may be, we go beyond personal will, receiving guidance from transpersonal will: the will of Self (as opposed to “self”).
Along that journey, however, people can fail to execute our will in a way which allows our goals to be realised. This post looks at the aspects of will, which, if they are not employed or are employed badly, can stunt the client’s intentions, keeping their goals from ever realising.
Aspects of will: Strength, Skill, and Virtue
Strength
When people make statements as mentioned above, decrying their lack of “will power” or “internal energy”, they are probably referring to the most well-known aspect of will: that is, “strong will”. It is believed that when we are born, we are unaware that we are separate from our birth giver. The beginning of individuation (the process of forming a stable personality) is the beginning of recognising that “will” exists. We are not only separate from Mum; we actually want something other than what Mum seems to be giving us. We come to see that we have arms and legs and a mouth, so we use these tools to explore the world the way we want to. We learn that crying will have certain needs met. It is the aspect of “strong will” that ensures that our willed act — say, crying for food — contains enough intensity or “drive” to carry out its purpose (getting us fed).
In other words, have you ever seen a really hungry baby stop crying after a very short time if it is not fed? Generally, not. It is possible that our new diet or exercise regime has failed because we didn’t elicit the intensity or “drive” to the intention to exercise or stick to our new diet. We may need to explore what situations in life are keeping us from applying greater intensity to the question. Maybe our desire to change is not worth the requisite “will” or “energy”. The road of least resistance is very common as we age and accumulate more life responsibilities.
This is not true for everyone. Some people will vehemently proclaim that do want to change. It is not lack of wanting, or lack of “will”. What is missing may be the second aspect of “will”, equally important to the first: that of skilful will.
Skill
Several sayings are relevant here:
- Environment is stronger than will power.
- When imagination and will power go up against one another, imagination wins every time.
These axioms allude to the often-unrecognised reality that we cannot generally achieve our goals through strong will, alone. Consider the alcoholic who desperately wants to stop drinking but they continue relapsing. If we put our will into competition with other psychological forces — such as impulse or feeling — it becomes overwhelmed; we end up stressed without accomplishing our goal. What we are missing in this case is likely to be the capacity to develop strategy, approaching the goal skilfully, and practically. Oftentimes, we want to achieve our goal without attaining the skills necessary to achieve it.
If you want to lose weight, for example, could think that you simply need to eat fewer calories and the extra kilo’s will start dropping off. Calories in Vs Calories out. But your role as strategist can be very helpful if you establish, for example, whether you’re often in situations where controlling food intake is difficult: say, when going out to eat or eating at private parties, or it’s the holiday like Christmas. Are you eating balanced meals, with sufficient protein (for example) to sustain yourself? Are you getting enough sleep to avoid overproduction of the hunger-inducing hormone ghrelin? How much do you know about body composition, the endocrine system, metabolism, nutrition, and exercise physiology?
There are myriad ways to be skilful around weight loss plans, and you may need to consider adopting some of them for success. For example, do you have effective interpersonal skills to communicate your needs to the people in your life that exercise and healthy eating is valuable to you, and you need their support? Or do you have the skills to join a peer group that exercises regularly. Perhaps you could improve your financial skills to budget for a Personal Trainer.
If we must merely “strong-arm” ourselves to achieve every end, we end up exhausted and discouraged, with few accomplishments. “Skilful will” allows us to use will not as a direct power or force, but as a function which stimulates, regulates, and directs other functions of ourselves so that they lead to the goal. For example, learning mindful eating skills may cultivate a relationship with bodily sensations which allows you to observe the sensation of true hunger pains as opposed to times when you eat because of boredom or wanting to feel good (temporarily). You can also learn skills to meet alleviate boredom or feeling emotionally nourished in other ways.
Even with employing strong and skilful will, however, your may not achieve your goal(s). That’s okay. Please do not judge yourself. It’s what Buddhism called the second arrow. That is, you already didn’t meet your goal (the first arrow) and then you judge yourself for it (the second arrow). You are human, not superhuman.
A third aspect, equally important with the first two, may also need to be employed. It is “Virtuous Will”.
Virtue
Is your goal something you can achieve all by yourself through prudent use of strong and skilful will? No one is an island; we all live in communities and interact with family, friends, co-workers, gym instructors, enemies, and others on a regular basis. Those willed acts that succeed in accomplishing the will-er’s goal do so because they have considered the need to choose goals that are consistent with the welfare of others and the common good of humanity. They also must be consistent with “virtuous will” to the “self”.
The bottom line here is that many people need to do serious work around having virtuous will for themselves. For example, if you “hate” yourself for weighing more than what you would like, the motivation for change is unlikely to succeed because it is born in self-hatred. It is more effective to improve your self-esteem and sense of worth as a person, independent of your goal, so that any weight loss and subsequent weight maintenance can be in the context of “something I do to value myself; I like myself as I am and want to enhance the health of that self”.
Accessing transpersonal will
According to Roberto Assagioli, the founder of Psychosynthesis, using our will doesn’t stop with developing strong, skilful, and virtuous will: the three aspects of personal will. Assagioli claims that we can manifest all three of those and still be unhappy if we do not see how our personal goals align with something greater than ourselves. Having that solid sense of meaning and purpose to achieve something beyond the benefit of our little “self” helps us to reach beyond the limitations of ordinary consciousness to more expanded, intense states of awareness.
To yearn for that and not have it is what Viktor Frankl called “the abyss experience”: the opposite of Maslow’s peak experience (Boeree, 2006). Yet it is often in the abyss and despair of meaninglessness that we feel the pull of the superconscious, activating our transpersonal will and giving us access to another level of being. And then life becomes more interesting, as we try to balance the needs of material life (our immanence) and those of our higher levels of being (our transcendence), experienced as intentions arising from our transpersonal will.
Even the hypothetical person’s goal of weight loss (seemingly a very personal goal) may be able to access transpersonal will. Let’s say you lose the weight, arriving at your goal weight. You may enjoy a slender new body for a while, but ultimately that may not be enough to sustain lasting contentment, peace, and satisfaction. Looking “good” may not be the sole purpose of the original intention. If you can transform your goal, however, to a goal more inclusive of potential good for humanity as a whole — you may find that your personal will is aligned with transpersonal will. Just look at all the people on Youtube trying to help others, or the reward and continued sobriety members of Alcoholics Anonymous are given by “helping others”. Transpersonal will goes beyond the self and comes back to support our intention. Perhaps you want to write about healthy-body image as a method to transcend your Will to others.
The Will and the End of this Article
An effective and intentional use of will increases joy, openheartedness, and equanimity. Through use of not only strong will, but also skilful and good will — and perhaps even transpersonal will — your New Year’s resolutions will be far more likely to succeed, and you can experience willing as an act that leads to joy.
References
- Assagioli, R. (1973/1984). The act of will: A guide to self-actualization and self-realization. Wellingborough: Turnstone Press.
- Boeree, C. G. (2006). Viktor Frankl. Personality theories. Shippensburg University. Retrieved on 5 November, 2012, from: Website.
- Mental Health Academy. (n.d.). Understanding Will. Mental Health Academy.
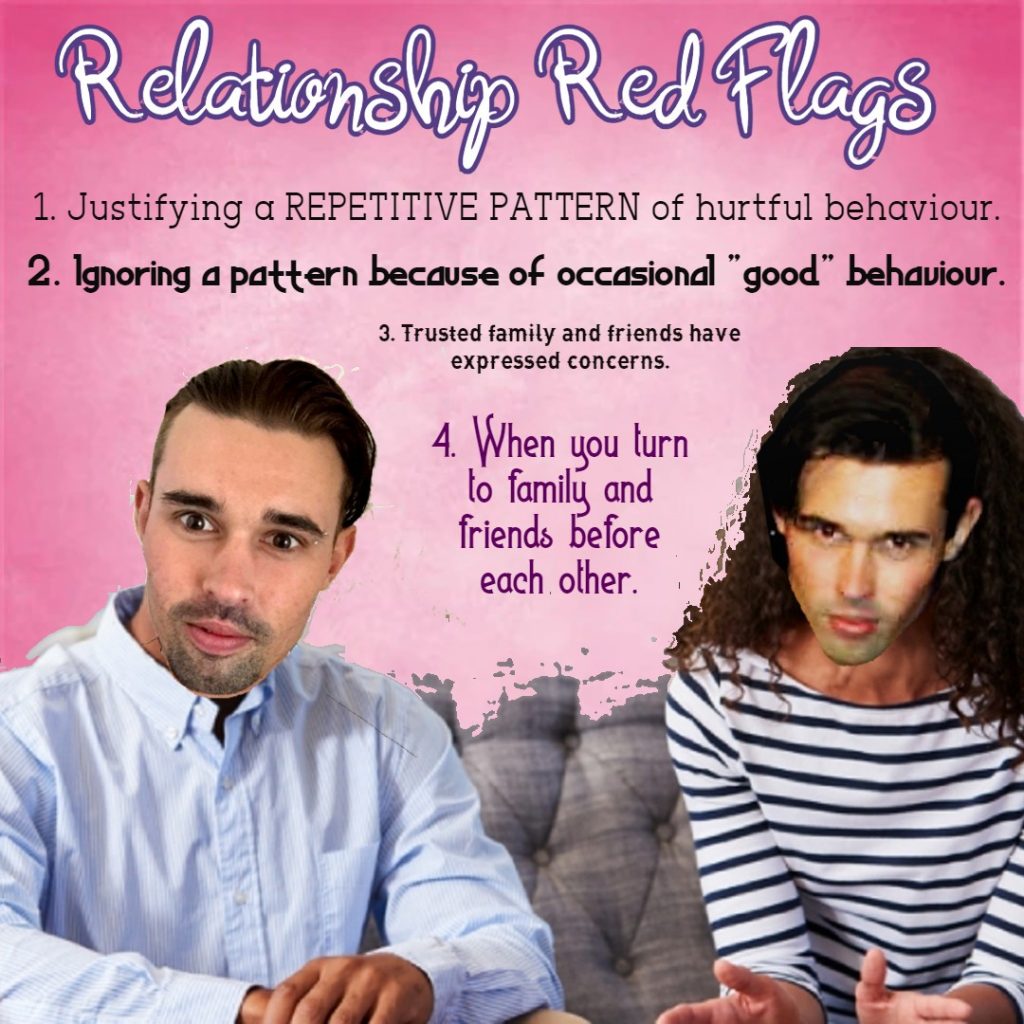
If we’re honest with ourselves, we know if a relationship isn’t working, if it is abusive or hurtful, or if it has run it’s course. We can ask trusted family and friends for their opinion if we’re confused or unsure.If we’re honest with ourselves, we know if a relationship isn’t working, if it is abusive or hurtful, or if it has run it’s course. We can ask trusted family and friends for their opinion if we’re confused or unsure.
Domestic Violence line (24 hours) 1800 65 64 63
Domestic violence services and support contact list | Family & Community Services (nsw.gov.au)