Category: Uncategorized
Fact. Truth. Belief. They are related but distinct. Here’s a clear explanation showing how they differ and interact:Fact. Truth. Belief. They are related but distinct. Here’s a clear explanation showing how they differ and interact:
1. Fact
Definition:
A fact is something that is objectively real and can be proven to be true. It exists independently of what anyone thinks or believes.
Example:
- It is a fact that Australia is in the Southern Hemisphere.
Key Points:
- Facts don’t change based on opinion.
- They can be verified with evidence (e.g. scientific data, observation, reliable records).
- Facts are the foundation upon which truth claims and beliefs can be tested.
2. Truth
Definition:
Truth is a quality of a statement or belief that accurately reflects reality or fact.
Example:
- “Australia is in the Southern Hemisphere” is a true statement because it corresponds with the fact.
Key Points:
- Truth depends on alignment with facts.
- Truth is often expressed in language or claims (“That’s true”, “That’s not true”).
- Something can be true even if no one believes it (e.g. the Earth orbited the Sun even when most people thought otherwise).
3. Belief
Definition:
A belief is something a person thinks or accepts as true, whether or not it actually is.
Example:
- Someone might believe that kangaroos can be kept as pets in all Australian states — but that belief isn’t necessarily true or factual.
Key Points:
- Beliefs are subjective — they vary between individuals and cultures.
- A belief can be true or false, depending on whether it aligns with facts.
- People often act based on their beliefs, regardless of whether they are accurate.
How They Interact
- A belief can be true or false:
→ If your belief aligns with fact, it’s true.
→ If not, it’s false — even if sincerely held. - Truth depends on fact:
→ A statement is true if it correctly describes a fact. - Facts stand alone:
→ They are not changed by belief or opinion.
The phrase “Say what you mean, but don’t say it mean” is all about the balance between honesty and kindness in communication.
Here’s what it means:
- “Say what you mean”:
Be clear and truthful. Express your real thoughts and feelings. Don’t beat around the bush or pretend to agree when you don’t. - “But don’t say it mean”:
Speak with kindness and respect. Even when you’re being honest or giving criticism, there’s no need to be rude, hurtful, or aggressive.
Why it matters:
This phrase promotes healthy communication. It’s a reminder that:
- You can be honest without being harsh.
- Tone and delivery matter just as much as the words.
- Empathy and respect should guide your conversations—even when it’s hard.
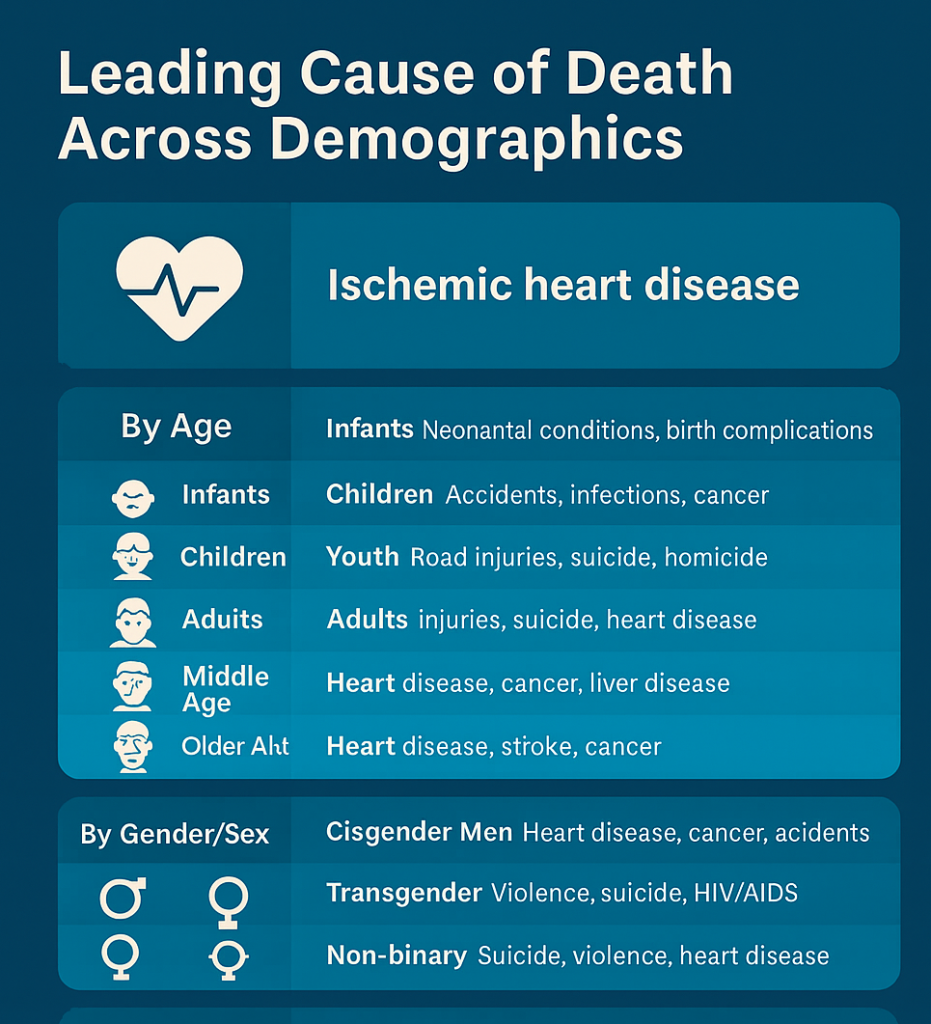
Overall Global Leading Cause of Death
- Ischemic heart disease (coronary artery disease) – Still the #1 cause of death worldwide.
- Followed by: Stroke, chronic obstructive pulmonary disease (COPD), lower respiratory infections, and cancer (e.g., lung, liver, colorectal).
Breakdown by Category
By Age
| Age Group | Leading Cause(s) of Death |
|---|---|
| Infants (<1) | Neonatal conditions, birth complications, infections |
| Children (1–14) | Accidents (injuries), infections (low-income countries), cancers (e.g., leukemia) |
| Youth (15–24) | Road injuries, suicide, homicide (varies by country) |
| Adults (25–44) | Injuries (road, drug overdose), suicide, HIV/AIDS (in some countries), heart disease |
| Middle Age (45–64) | Heart disease, cancer (esp. lung, colorectal, breast), liver disease |
| Older Adults (65+) | Heart disease, stroke, cancer, Alzheimer’s disease |
By Gender/Sex
| Group | Leading Cause of Death |
|---|---|
| Cisgender Men | Heart disease, cancer (lung, liver), accidents |
| Cisgender Women | Heart disease, cancer (breast, lung), stroke |
| Transgender Individuals | Elevated risk from violence, suicide, and HIV/AIDS (especially trans women of color); limited large-scale data |
| Non-binary | Insufficient population-specific data, but risks often parallel those of trans populations or assigned sex at birth |
By Race/Ethnicity (Example: United States)
| Group | Top Causes | Unique Issues |
|---|---|---|
| White (non-Hispanic) | Heart disease, cancer, drug overdose | |
| Black or African American | Heart disease, cancer, higher stroke risk | |
| Hispanic/Latino | Heart disease, cancer, diabetes | |
| Native American | Accidents, liver disease, diabetes, suicide | |
| Asian American | Cancer (leading cause), stroke, heart disease |
Note: Disparities arise from systemic inequalities, access to care, and social determinants of health.
By Sexuality (LGBTQ+)
- Limited global data, but in many regions:
- Higher risk of suicide, mental health disorders, substance abuse, HIV/AIDS (especially among MSM and trans women).
- Discrimination and healthcare avoidance contribute to worsened outcomes.
- Common causes of death still include heart disease and cancer, with higher rates of premature death linked to stigma and healthcare disparities.
By Geographic Region
| Region | Leading Cause(s) |
|---|---|
| High-Income Countries | Heart disease, cancer, Alzheimer’s, stroke |
| Low- and Middle-Income Countries | Infectious diseases (TB, HIV), maternal mortality, stroke, heart disease |
| Africa | HIV/AIDS, malaria, lower respiratory infections |
| Asia | Stroke, heart disease, chronic lung disease |
| North America | Heart disease, cancer, drug overdose (opioid crisis) |
| Europe | Heart disease, stroke, cancer |
| Latin America | Violence (in younger adults), heart disease, diabetes |
By Profession
- Agricultural/farm workers: High injury rates, pesticide exposure, suicide
- Construction workers: Falls, injuries, exposure to toxins (e.g., asbestos)
- Healthcare workers: Infectious disease, burnout, mental health risks
- Military/first responders: Combat-related injuries, PTSD, suicide
- Office workers: Sedentary lifestyle risks (heart disease, diabetes)
Occupation-linked deaths often relate to environmental exposures, physical risks, or psychological stressors.
Conclusion:
Across almost all demographics, heart disease remains the leading cause of death, followed by cancer, stroke, and—in certain populations—accidents, suicide, or infectious diseases. However, the underlying causes (social, economic, political) differ significantly based on identity, geography, and profession.
Would you like this formatted into a chart, infographic, or specific to a country or report you’re working on?
Thinking About Change? How Motivational Interviewing Can HelpThinking About Change? How Motivational Interviewing Can Help
If you’ve ever found yourself thinking “Part of me wants to change… but part of me’s not sure”, you’re not alone. That back-and-forth, weighing things up—“Should I? Shouldn’t I?”—is a normal part of how people process big (and small) decisions. In counselling, this is called ambivalence, and rather than seeing it as a barrier, Motivational Interviewing (MI) treats it as a starting point for meaningful conversations.
What Is Motivational Interviewing?
Motivational Interviewing is a counselling approach that helps people explore their own reasons for change, without pressure or judgment. It’s a respectful, supportive way of helping you work through the push-pull that often comes with making decisions. You’re in the driver’s seat—we’re just here to help you navigate.
You might hear MI described in different ways:
In simple terms:
“MI is a collaborative conversation style that helps strengthen your own motivation and commitment to change.”
In practice:
“MI is about helping you make sense of mixed feelings and explore what’s right for you—based on your values, your goals, and your life.”
MI isn’t about telling you what to do. It’s about listening deeply, asking thoughtful questions, and helping you make sense of where you’re at—and where you might want to go.
Why It’s Not Just a Quick Fix
While MI can be used in short sessions, the research shows it works best when there’s time to really explore your thinking. In studies where people had just one 15-minute session, the outcomes were decent. But when they had more time—say, several sessions of an hour—the results were much stronger. That’s probably because real change often takes time, reflection, and a bit of back-and-forth.
MI originally started in the health world—helping people reduce alcohol use, manage weight, or improve their health. More recently, it’s been used to address things like vaccine hesitancy. But MI isn’t just for health issues. It can also help with things like relationship struggles, career decisions, or anything where you might feel stuck or unsure.
Ambivalence Is Normal
Let’s say you’re thinking about quitting smoking, leaving a relationship, or starting something new. You might feel torn—part of you is ready, and another part isn’t. That’s ambivalence.
MI offers tools to help with this, including something called the Decisional Balance, which simply helps you look at both sides: What are the good things about staying the same? What are the reasons you might want to change?
But here’s the thing—MI isn’t about pushing you toward a particular outcome. If you’re trying to make a decision where there’s no obvious “right” answer—like whether to stay in a relationship—the counsellor stays neutral. They don’t steer you in one direction. Instead, they help you explore what matters to you.
Talking Your Way Toward Change
One of the interesting things about MI is how it pays attention to the language you use when you talk about change.
Some of the things people say when they’re starting to think about change include:
- “I probably should cut down…”
- “I’d like to feel better about this…”
- “I don’t know if I can keep doing this…”
These kinds of statements are called change talk—and they’re actually signs that something inside you is shifting. MI aims to gently encourage and grow this kind of talk, because research shows that the more someone talks about change, the more likely they are to act on it.
There’s also sustain talk, which sounds like:
- “I don’t smoke that much…”
- “I know I should, but it helps me relax.”
- “Now’s not really the right time.”
Both are normal. In MI, there’s no need to rush. Instead, the focus is on listening to both sides of you—and helping you get clearer about what you want to do next.
Getting Skilled Support
Like any professional approach, MI works best when the counsellor is trained and skilled in using it. Some practitioners have their sessions reviewed (with consent) by independent experts to make sure the spirit and skills of MI are being used well.
If you ever hear a practitioner say they “do MI”, you can ask what that looks like. The most effective use of MI goes beyond just asking open-ended questions or offering summaries—it’s about how your counsellor supports you in finding your own reasons for change.
What a Session Might Involve
Motivational Interviewing tends to follow a flexible process with four key parts:
- Engaging – Building trust and understanding
- Focusing – Exploring what matters most to you
- Evoking – Drawing out your own reasons for change
- Planning – When you’re ready, looking at possible next steps
You don’t have to go through these in a straight line. Some days you might focus on one step, then circle back to another later. It’s all guided by you—your pace, your readiness, your goals.
In Summary
If you’re feeling uncertain about making a change—or you’ve been thinking about it for a while but haven’t quite landed on what to do—Motivational Interviewing could be a really helpful way to explore things.
It’s not about being told what to do, and it’s not about “fixing” you. It’s a respectful, evidence-based approach that helps people work through their own ambivalence, connect with what matters to them, and move toward change when they’re ready.
Change doesn’t have to be instant. And it doesn’t have to be perfect. But it can start with a conversation.
Suicidality: Talking About Suicide and SupportSuicidality: Talking About Suicide and Support
Supporting someone who’s having thoughts of suicide is one of the most important, and at times most challenging, parts of a support persons role. People who experience suicidality can vary from passing ideas to serious planning and often come from a place of deep emotional pain. We all have a duty to respond with care, compassion, and an attempt to understand the experience in a way that keeps safety at the heart of every conversation.
Firstly, if you or someone you know is having thoughts of suicide, please know that you’re not broken or beyond help. These thoughts often come when emotional pain feels unbearable and we can’t see a way out. But things can shift, and help is available. We may spend much of our time alone, and we can feel alone even in a crowded room, but you are not alone in this. Suicidality is not uncommon.
The Numbers Today
According to the latest figures (ABS, 2023):
Suicide is the leading cause of death for Australians aged 15 to 44.
In 2022, over 3,100 people died by suicide—about 8.6 deaths each day.
Men account for 75% of those deaths, though women attempt suicide more often (but less often fatally).
According to the Black Dog Institute, roughly 65,000 Australians attempt suicide each year, while around 3,200 die by suicide annually.
Rates among Aboriginal and Torres Strait Islander peoples are more than double the national average.
People living in rural and remote areas face higher suicide risks due to isolation, limited services, and other pressures.
Why Does the Mind Think About Suicide?
From a humanistic psychology point of view, suicidal thoughts are not signs of illness or failure, they are a deep emotional signal that something in your life or environment needs care, change, or healing.
Each person and living creature on the planet are inherently worthy, with an innate drive to survive, grow, connect, and for humans, find meaning. When life feels full of suffering, such as grief, isolation, trauma, shame, or hopelessness, the mind may start to believe that death is the only way to stop the pain.
In this view, suicidal thoughts are often not about wanting to die—but about wanting the pain to stop.
They arise when:
You feel disconnected from others or from yourself.
You feel stuck in circumstances that seem unchangeable.
You believe your worth or purpose has been lost.
You’re exhausted from holding on or pretending you’re okay.
But the humanistic perspective also holds this powerful truth: you are more than your pain, and within you is a capacity for healing, choice, and change, even if it doesn’t feel like it right now.
Treat Yourself with Compassion, Not Criticism
It’s easy to get caught in a spiral of self-blame. But you are not weak or selfish. You are a human being who is hurting—and just like you wouldn’t shame someone for being in physical pain, you deserve the same care when your pain is emotional.
Ask yourself:
If someone I loved felt this way, what would I want them to know?
Then try to offer yourself the same kindness.
Reach Out – Connection Saves Lives
Talking to someone can ease the intensity of what you’re feeling. You don’t have to explain everything. Just saying, “I’m not okay right now,” is enough to start.
Lifeline 13 11 14
Beyond Blue 1300 22 4636
Suicide Call Back Service: 1300 659 467
Beyond Blue: 1300 22 4636
13YARN (Support for Aboriginal and Torres Strait Islander Peoples): 13 92 76
QLife – National LGBTQIA+ Peer Support and Referral Service: 1800 184 527
Hours: 3pm – Midnight (local time), every day
What they offer: Confidential, non-judgemental, and inclusive support from trained LGBTQIA+ peer workers. They are not a crisis line like Lifeline, but they can support people in distress and connect you with further help if you’re at risk.
How Counselling Can Help: Evidence-Based Approaches
Counsellors and Psychologists don’t rely on guesswork when helping someone who’s feeling suicidal. They use researched strategies to support recovery. Here are a few key approaches:
Collaborative Assessment and Management of Suicidality (CAMS): This method focuses on working together with the person in distress, rather than telling them what to do. It aims reduce suicidal thoughts more effectively than traditional therapy.
Cognitive Behavioural Therapy for Suicide Prevention (CBT-SP): This version of CBT focuses specifically on managing suicidal thoughts by teaching problem-solving and positive thinking strategies.
Dialectical Behaviour Therapy (DBT): Originally designed for people with intense emotions or borderline personality disorder, DBT is now widely used to reduce suicide risk by teaching emotional regulation, mindfulness, and better relationship skills.
Safety Planning: This involves creating a personalised plan for what someone can do when they feel at risk, including who to call, calming strategies, and safe places to go.
Means Restriction Counselling: This involves helping someone reduce their access to anything they might use to harm themselves, like certain medications or weapons, done through sensitive, respectful conversations.
Barriers to Speaking Up
Even with growing public awareness, there’s still a strong stigma around suicide. Many people worry they’ll be judged, locked up, or shamed if they admit they’re struggling. These fears can stop people from reaching out for help, which is why creating a safe, non-judgmental space is so important in counselling.
Rural and Remote Communities
People in regional and remote parts of Australia often find it harder to access mental health support. Telehealth (online or phone sessions) has helped bridge that gap, but it’s not always easy to pick up on non-verbal cues or respond to crises from a distance.
Cultural Awareness Matters
For Aboriginal and Torres Strait Islander peoples, suicide cannot be separated from the impacts of colonisation, loss of culture, and ongoing trauma. Culturally safe, community-led solutions are essential and more effective in these contexts.
Remember That Feelings Change—Even the Darkest Ones
It may not feel like it right now, but these feelings will pass. Emotions are like waves—sometimes crashing, sometimes calm—but never permanent.
What you feel today is not a life sentence. With support and time, things can change. You deserve the chance to see what healing and hope feel like.
Safe Haven NSW Services (for suicidal distress, NOT EDs)
Please check official websites for update information re contact information, hours of operation, and status of operation i.e., still operating. The information on this website has been collected June 2025.
Safe Havens are calm, non-clinical spaces where you can talk with peer workers and mental health clinicians if you’re in emotional crisis — no appointment needed.
No police or emergency involvement unless requested or necessary.
Warm, trauma-informed and recovery-focused.
🔗Find your local Safe Haven: nsw.gov.au/mental-health-initiatives/safe-haven
Examples:
Safe Haven locations across NSW — these are welcoming, non-clinical places where anyone feeling suicidal or in deep distress can drop in and speak to peer workers or mental health clinicians. No appointment, referral, or Medicare card needed. Visit the following for operating hours and locations across NSW: Safe Haven
Regional & Metro Locations
Campbelltown / Ambarvale (SWSLHD)
Address: 80 Woodhouse Drive, Ambarvale (Campbelltown area)
Open Mon, Fri, Sat, Sun 2 – 9 pm
Phone: 0457 093 109 during hours swslhd.health.nsw.gov.au
North Ryde (Macquarie Hospital)
For youth aged 12–17 (sometimes to 18 if still at school)
Open daily 4 – 8 pm and public holidays nslhd.health.nsw.gov.au
Parramatta / Westmead
Drop-in at 26 Grand Ave, Westmead
Open Sun–Wed 3:30 – 9:30 pm
Phone: 0436 377 113
Bega Safe Haven, Bega, NSW, Australia, Supports 14 + in a calm, welcoming space.
Broken Hill Safe Haven, Broken Hill, NSW, Australia, Supports 17 + with peer and clinician support
Brookvale Safe Haven, Brookvale, NSW, Australia, High‑school aged young people support
Darlinghurst, NSW, Australia, 16 + LGBTQIA+ inclusive spot at St Vincent’s
St Vincent’s O’Brien Centre, 390 Victoria Street, Darlinghurst NSW 2010
Hours: Monday: closed, Tuesday: closed, Wednesday: 5:00pm – 8:30pm, Thursday: 5:00pm – 8:30pm, Friday: 5:00pm – 8:30pm, Saturday: 12:00pm – 4:00pm, Sunday: 12:00pm – 4:00pm.
Gosford Safe Haven, General adult Safe Haven
Corner of Ambulance Road and Holden Street, Gosford NSW 2250
Hours: Monday: 9:00am – 4:30pm, Tuesday: 9:00am – 4:30pm, Wednesday: 9:00am – 4:30pm, Thursday: 9:00am – 4:30pm, Friday: 9:00am – 4:30pm, Saturday: closed, Sunday: closed, Closed on public holidays
Phone: (02) 4394 1597
Kogarah Safe Haven, Kogarah, NSW, Australia,16 + adults,
U2/15 Kensington St, Kogarah NSW 2217
Phone: (02) 9113 2981
Predicting behaviour: Social Psychological Models of BehaviourPredicting behaviour: Social Psychological Models of Behaviour
Social psychological models of behaviour attempt to explain why individuals act the way they do in various social contexts. These models integrate individual, interpersonal, and societal factors to provide insights into behaviour. Here’s an overview of some key models:
1. Theory of Planned Behaviour (TPB) proposes that behaviour is influenced by:
– Attitudes toward the behaviour
– Subjective norms (perceptions of others’ approval)
– Perceived behavioural control (i.e., confidence in one’s ability to perform the behaviour [self-efficacy])
2. Social Cognitive Theory (SCT) suggests that behaviour is the result of:
– Reciprocal interaction between personal factors (beliefs, attitudes), environmental factors (social norms), and behaviour itself
– Concepts like self-efficacy (belief in one’s ability) play a major role.
3. Health Belief Model (HBM), designed to predict health-related behaviours. Behaviour is driven by factors such as perceived:
– Susceptibility (risk of harm)
– Severity (consequences of harm)
– Benefits (advantages of action)
– Barriers (obstacles to action)
4. Cognitive Dissonance Theory explains how people strive for consistency between their beliefs, attitudes, and behaviours. When inconsistency arises, they feel dissonance (mental discomfort) and are motivated to reduce it by changing their attitudes or actions.
5. Social Identity Theory examines how individuals define themselves within social groups. Behaviour is influenced by group membership, including in-group favouritism and out-group bias.
6. Attribution Theory focuses on how people explain their own and others’ behaviours. Explains behaviour as being attributed either to internal (dispositional) or external (situational) factors. For example, it is common for people to attribute negative outcomes in their life to external factors rather than internal factors.
7. Elaboration Likelihood Model (ELM) explains how people process persuasive messages and what determines whether those messages will change attitudes or behaviour. It’s often applied in areas like marketing, communication, and public health campaigns. The ELM identifies two primary routes through which persuasion can occur:
– Central Route; this route involves deep, thoughtful consideration of the content and logic of a message. People are more likely to take the central route when they are motivated to process the message (e.g., the topic is personally relevant or important to them) and they can understand and evaluate the arguments (e.g., they aren’t distracted, and they have enough knowledge about the subject). Persuasion through the central route tends to result in long-lasting attitude change that is resistant to counterarguments. Example: A person researching the pros and cons of electric cars before deciding to buy one.
– Peripheral Route, which relies on superficial cues or heuristics (mental shortcuts) rather than the message’s content. People are more likely to take the peripheral route when they are not highly motivated or lack the ability to process the message deeply, and when they focus on external factors like the attractiveness or credibility of the speaker, emotional appeals, or catchy slogans. Persuasion through this route tends to result in temporary attitude change that is less resistant to counterarguments. Example: A person choosing a product because their favourite celebrity endorsed it.
8. Self-Determination Theory (SDT) emphasizes intrinsic and extrinsic motivation. It emphasizes the role of intrinsic motivation—doing something for its inherent satisfaction—over extrinsic motivation, which is driven by external rewards or pressures. It suggests that behaviour is influenced by the need for:
– Autonomy (control over one’s actions); When people perceive they have a choice and are acting in alignment with their values, their motivation and satisfaction increase.
– Competence; Refers to the need to feel effective, capable, and successful in achieving desired outcomes. People are motivated when tasks challenge them at an appropriate level and provide opportunities for growth and mastery. Example: A gamer progressing through increasingly difficult levels, gaining skills and confidence along the way.
– Relatedness; Refers to the need to feel connected to others and experience a sense of belonging. Supportive relationships and positive social interactions enhance motivation and well-being. Example: Employees feeling a bond with their colleagues in a collaborative work environment.
9. Social Learning Theory proposes that behaviour is learned through observation and imitation. Role models and reinforcement play a key role in shaping actions.
10. Transtheoretical Model (Stages of Change) explains behaviour change as a process occurring in stages: precontemplation, contemplation (ambivalence), preparation, action, and maintenance
These models provide frameworks to understand behaviours in contexts like health, decision-making, group dynamics, and social influence.
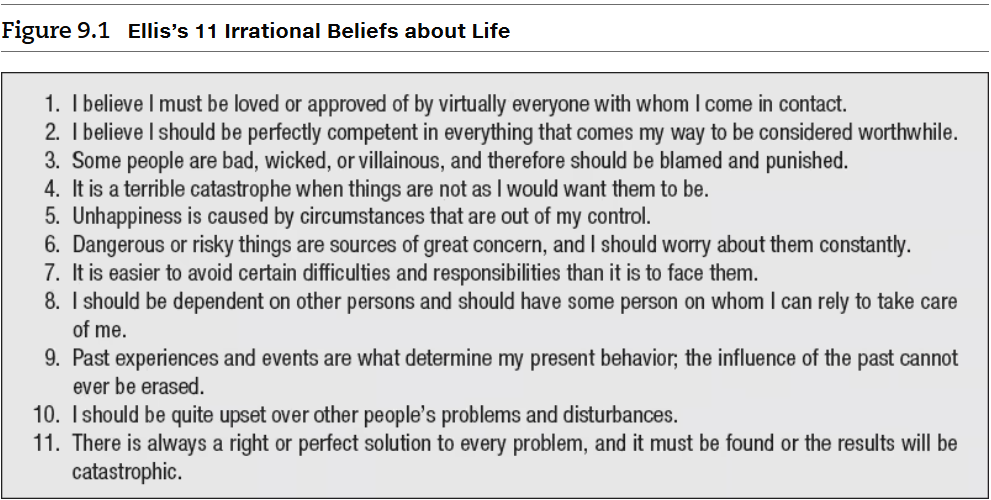
Albert Ellis’s “Irrational Belief’s about Life” and Self-stereotypingAlbert Ellis’s “Irrational Belief’s about Life” and Self-stereotyping
Albert Ellis, in his Rational Emotive Behaviour Therapy (REBT), identified a number of dysfunctional beliefs that people often hold. Ellis intentionally adopts extreme views to emphasize how people often exaggerate their perspectives irrationally. He referred to this tendency as “awfulizing,” where we negatively overgeneralise situations. This behaviour can stem from a strong desire for certainty, causing us to perceive things in extreme terms rather than viewing them as part of a nuanced spectrum. Consequently, this leads to the formation of self-stereotypes.
A self-stereotype refers to the process of applying generalised beliefs or stereotypes about a group to oneself, especially when one identifies as part of that group. For instance, if someone belongs to a specific cultural or social group (gay men) and internalises the commonly held stereotypes about that group (partying and casual sex), they may unconsciously start viewing and behaving in ways that align with those generalisations.
Effective strategies and techniques for moderate to intense anxiety:Effective strategies and techniques for moderate to intense anxiety:
Managing moderate to intense anxiety often involves a combination of techniques that address both the mind and body. Here are some effective strategies:
1. Breathing Exercises: Practice slow, deep breathing to calm your nervous system. For example, inhale for a count of four, hold for four, and exhale for four.
2. Progressive Muscle Relaxation: Tense and then relax each muscle group in your body, starting from your toes and working upward.
3. Grounding Techniques: Use the 5-4-3-2-1 method to focus on your senses—identify 5 things you see, 4 you feel, 3 you hear, 2 you smell, and 1 you taste.
4. Mindfulness and Meditation: Engage in mindfulness practices to stay present and reduce anxious thoughts. Apps like Headspace or Calm can be helpful.
5. Physical Activity: Exercise, even a short walk, can release endorphins and reduce anxiety levels.
6. Cognitive Behavioural Techniques: Challenge negative thoughts by questioning their validity and replacing them with more balanced perspectives.
7. Healthy Lifestyle Choices: Maintain a consistent sleep schedule, eat nutritious meals, and limit caffeine and alcohol intake.
8. Journaling: Write down your thoughts and feelings to process them and identify triggers.
9. Social Support: Talk to trusted friends, family, or support groups to share your experiences and gain perspective.
10. Professional Help: If anxiety persists, consider seeking therapy or counselling. Techniques like Cognitive Behavioural Therapy (CBT) or medication prescribed by a professional can be highly effective.
When traditional strategies don’t seem effective for managing intense, chronic anxiety, there are additional approaches you can explore:
a. Therapeutic Modalities:
Acceptance and Commitment Therapy (ACT): Focuses on accepting anxious thoughts rather than fighting them, while committing to actions aligned with your values.
Dialectical Behavior Therapy (DBT): Combines mindfulness with skills for emotional regulation and distress tolerance.
Eye Movement Desensitisation and Reprocessing (EMDR): Often used for trauma-related anxiety, it helps reprocess distressing memories.
b. Medication:
Anti-anxiety medications or antidepressants may be prescribed by a psychiatrist. These can help manage symptoms when therapy alone isn’t sufficient.
c. Lifestyle Adjustments:
Explore dietary changes, such as reducing sugar and processed foods, which can impact mood and anxiety levels.
Incorporate consistent physical activity tailored to your preferences.
d. Support Groups:
Joining a group for individuals with anxiety can provide a sense of community and shared understanding.
e. Intensive Programs:
Consider enrolling in an intensive outpatient program (IOP) or residential treatment program for anxiety, which offers structured and comprehensive care.
f. Emerging Treatments:
Research into treatments like ketamine therapy or transcranial magnetic stimulation (TMS) shows promise for treatment-resistant anxiety.
g. Alternative Therapies:
Practices like acupuncture, yoga, or tai chi can promote relaxation and reduce anxiety.
Biofeedback and neurofeedback can help you gain control over physiological responses to stress. They are techniques that help individuals gain control over certain physiological and mental processes. Here’s a breakdown:
i. Biofeedback is a mind-body therapy that uses sensors to monitor physiological functions like heart rate, muscle tension, breathing, or skin temperature. The goal is to provide real-time feedback to help individuals learn how to regulate these functions consciously. For example:
Heart Rate Variability Biofeedback: Helps manage stress by teaching control over heart rate.
Muscle Tension Biofeedback: Useful for conditions like chronic pain or tension headaches.
By practicing biofeedback, people can develop skills to manage stress, anxiety, and other health conditions2.
ii. Neurofeedback, a specialised form of biofeedback, focuses on brain activity. It uses electroencephalography (EEG) to monitor brainwaves and provides feedback to help individuals regulate their brain function. For instance:
It can help with conditions like ADHD, anxiety, depression, and PTSD.
During a session, individuals might watch visual cues or listen to sounds that reflect their brainwave activity, learning to adjust their mental state for better focus or relaxation4.
Both techniques are non-invasive and can be effective tools for improving mental and physical well-being.
IMPORTANT NOTE: It’s necessary to consult with a mental health professional or medical doctor to tailor these options to your specific needs.

