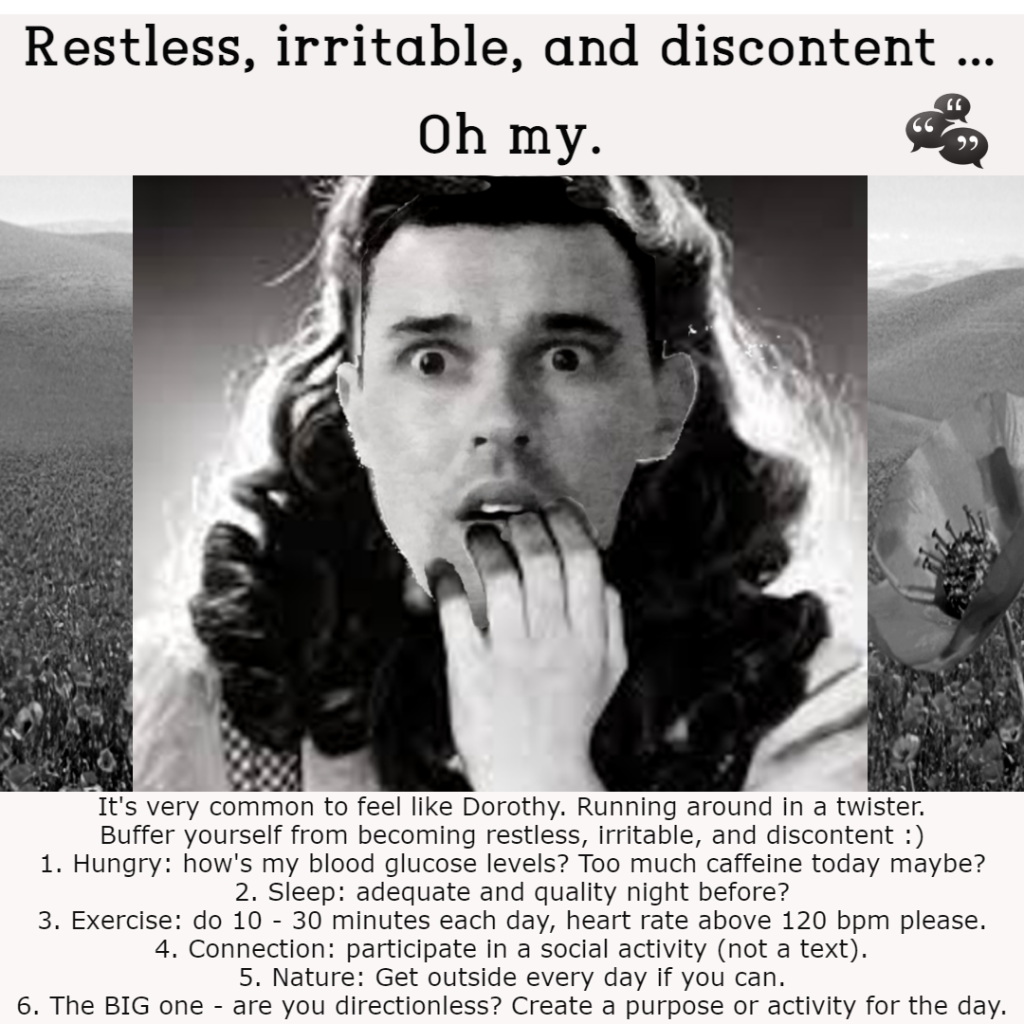
I would infer that you may be depleted in some area of your life. Generally, when I am having any of these experiences I can recognise that my basic needs, and possibly even transformative, needs are not met. My basic needs are food and water, adequate sleep, shelter and safety, social connection (belonging), and esteem needs (e.g., self-respect, self-worth, self-competence, mastery and achievement, integrity, sense of freedom and independence etc.). Perhaps only when all my deficiency needs are met, and I’m experiencing dissatisfaction with my growth needs, do I feel Restless, Irritable, and Discontent in this area of my life – however I assume some would argue that if I am feeling that way when attending to my growth needs, then I may have slipped back to Esteem Needs. You can look up Maslow’s Hierarchy of Needs for a visual representation if you like, using a search engine. Below is a GIF that I created to educate people on how we can buffer ourselves to vulnerabilities. It’s very telling to go into the body when we haven’t eat for a while, may be we’re running on caffeine, and you can feel the restlessness in the body. We have to fuel up when we’re hungry to buffer ourselves from becoming irritable and restless. If you’re feeling discontent with life, I would suggest a social activity, play time with friends, working on a project of some kind, or getting involved in your community.