I was recently browsing some of the units I completed for my counselling diploma – for revision. The human memory has not evolved to store, organise, categorise and recall all the large amounts of information we collect every day, nor is our memory always accurate. It’s important for counsellors and therapists to keep up to date with new approaches to counselling, and it doesn’t hurt to read over learned materials from college days. I thought I’d provide some learning about Acceptance and Commitment Therapy for readers.
Just to acknowledge the work of others, most of what is written below, I have retrieved and paraphrased from ACCEPTANCE AND COMMITMENT THERAPY Published by: Australian Institute of Professional Counsellors Pty Ltd.
Acceptance and commitment therapy, known as ACT (pronounced as the word ‘act’), is an approach to counselling that was originally developed in the early 1980s by Steven C. Hayes, and became popular in the early 2000’s through Hayes’ collaboration with Kelly G. Wilson, and Kirk Strosahl as well as through the work of Russ Harris. You can look them up on Youtube or Google if you’re interested in what they might have to say about ACT.
“Unlike more traditional cognitive-behaviour therapy (CBT) approaches, ACT does not
seek to change the form or frequency of people’s unwanted thoughts and emotions. Rather,
the principal goal of ACT is to cultivate psychological flexibility, which refers to the ability to
contact the present moment, and based on what the situation affords, to change or persist
with behaviour in accordance with one’s personal values. To put it another way, ACT
focuses on helping people to live more rewarding lives even in the presence of undesirable
thoughts, emotions, and sensations.”
(Flaxman, Blackledge & Bond, 2011, p. vii)
ACT interventions tend to focus around two main processes:
- Developing acceptance of unwanted private experiences that are outside of personal
control. - Commitment and action toward living a valued life (Harris, 2009)
In a nutshell, ACT gets its name from its core ideas of accepting what is outside of your personal control and committing to action that improves and enriches your life.
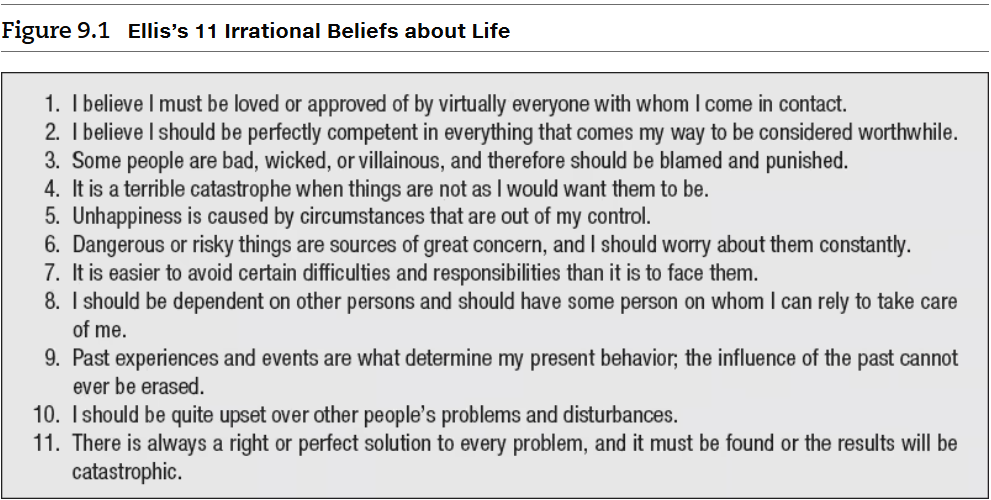
Cognitive Defusion is the process of learning to detach ourselves from our thought processes and simply observe them for what they are – “transient private events – an ever-changing stream of words, sounds and pictures” (Harris, 2006, p. 6). I think this component of ACT is incredibly beneficial if we practice it daily. I like to say, just like the function of the heart is to pump oxygenated blood around the body, one of the brain’s functions is to have thoughts. We can observe thoughts without taking them to mean more than what they are. Some thoughts are automatic, some are subconscious, and some are unconscious or preconscious beliefs that we consider to be true and factual and “rules” about how the world operates and how we have to operate in it. If someone is defused from their thought processes, these processes do not have control on the person; instead the person is able to simply observe them without getting caught up in them or feel the need to change/control them.
Acceptance is the process of opening oneself up and “making room for unpleasant feelings, sensations, urges, and other private experiences; allowing them to come and go without struggling with them, running from them, or giving them undue attention” (Harris, 2006, p. 7). Practicing acceptance is important because it encourages the individual to develop an ability and willingness to feel uncomfortable without being overwhelmed by it (Flaxman, Blackledge & Bond, 2011). It’s important to acknowledge that to accept something doesn’t mean we like it or have a passive attitude. It is to accept something exactly as it is and then we choose what to do with it. Think of the Serenity Prayer: Grant me the serenity to accept the things I cannot change, courage to change the things I can, and wisdom to know the difference.
Contact with the present moment is the concept of being “psychologically present” and bringing full attention to the “here-and-now” experience (Harris, 2009). I’d also argue that to psychologically present, we must also be aware of our physical body and the sensations within it and outside of it. Because we have the ability to think about the past and about the future, sometimes it can be difficult to stay in the present (Batten, 2011; Harris, 2009). Having contact with the present moment is essential because that it where we find out anchor and power. We have the ability to pay attention in a flexible manner to the present moment and connect with that experience rather than ruminate on past events or future possibilities (Lloyd & Bond, 2015). Some of you might say “What if I can’t stand the present moment?”. True. If you have extreme emotional experiences or have a history of trauma, it may be functional for you to use distraction or talking to someone when the present moment is “too much to take”. What we want to work towards is using healthy coping strategies in the present moment mindfully, instead of behaviours that no longer serve us.
Values, and identifying them, (i.e., what is important to the individual) is a central element of ACT because it assists clients to move in the direction of living and creating a meaningful life. One of the central goals of ACT is to help clients to connect with the things they value most and to travel in “valued directions” (Stoddard & Afari, 2014).
Committed action is the process of taking steps towards one’s values even in the presence of unpleasant thoughts and feelings (Harris, 2009). Behavioural interventions, such as goal setting, exposure, behavioural activation, and skills training, are generally used to create committed action. The ACT model acknowledges that learning is not enough, one must also take action to create change.
Self-as-context, or what I prefer to call “the observing self” or simply just our self-awareness, creates a distinction between the ‘thinking self’ and the ‘observing self’ (Harris, 2009). The thinking self refers to the self that generates thoughts, beliefs, memories, judgments, fantasies, and plans, whereas the observing self is the self that is aware of what we think, feel, sense, or do (Harris, 2009). “From this perspective, you are not your thoughts and feelings; rather, you are the context or arena in which they unfold” (Stoddard & Afari, 2014). Being aware of the observing self allows an individual to have a greater ability to be mindful and in the present moment, as they can separate themselves from the thoughts, beliefs, and memories they have.