Human-Kind. Isn’t that lovely. We have moved away from the patriarchal term mankind – ‘man’ who has not always been ‘kind’, necessarily – toward equality between the sexes and acknowledging gender fluidity. Noah touches on this. If you’re interested in the evolution of humanity and how we are capable of co-operating as a global community, give this book a go. You may experience information overload – but when condensing 2.4 million years into less than 500 pages, Harari goes alright. I’m someone who didn’t pay attention to history at school so I found this book enlightening, empowering and also disheartening at times. Harari writes about the breakthroughs of the Cognitive, Agricultural and Scientific Revolutions. The power of human imagination, math and language has been instrumental in the development of humankind into an apex predator, and the destruction of everything else.
Sapiens: A Brief History of Humankind.
Related Post
Polyvagal Theory and Trauma – Dr. Stephen PorgesPolyvagal Theory and Trauma – Dr. Stephen Porges
Stephen Porges, psychiatry professor and researcher, on the polyvagal theory he developed to understand our reactions to trauma:
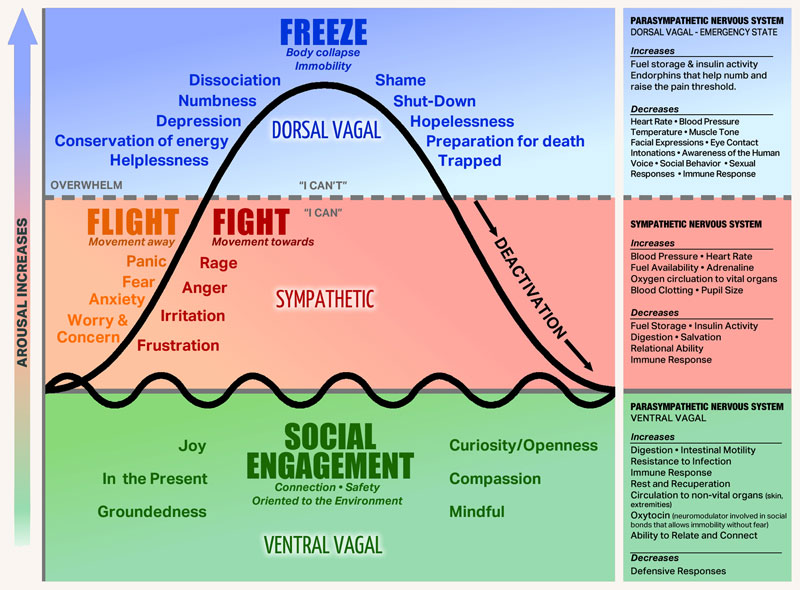
[Paraphrased] Polyvagal theory articulates three branches of the autonomic nervous system (ANS) that evolved from primitive vertebrates to mammals. First, there is a system known as ‘freeze’, which involves death feigning or immobilisation. Second, the ANS has a ‘fight or flight’ system, which is a mobilisation system. And third, with mammals, there is what Porges calls, a social engagement system (SES), which can detect features of safety, and actually communicate them to another. The SES may also be referred to by some as ‘rest and digest’, which Porges theory suggests is a function of the Vagus Nerve – the tenth cranial nerve, a very long and wandering nerve that begins at the medulla oblongata. When an individual experiences feelings of safety (within an SES state), the autonomic nervous system can support health restoration. In terms of dealing with a life threat, an ordinary person will most likely go into a feigning death, dissociative state of ‘freeze’.
Polyvagal theory in psychotherapy offers emotional co-regulation as an interactive process between therapist and client which engages the social engagement system of both therapist and client. Social engagement provides experiences of safety, trust, mutuality and reciprocity in which we are open to receiving another person, just as they are.
The following extract has been retrived from https://www.theguardian.com/society/2019/jun/02/stephen-porges-interview-survivors-are-blamed-polyvagal-theory-fight-flight-psychiatry-ace
Polyvagal theory has made inroads into medical and psycho-therapeutic treatment, but how should it inform how people treat each other?
“When we become a polyvagal-informed society, we’re functionally capable of listening to and witnessing other people’s experiences, we don’t evaluate them. Listening is part of co-regulation: we become connected to others and this is what I call our biological imperative. So when you become polyvagal-informed you have a better understanding of your evolutionary heritage as a mammal. We become aware of how our physiological state is manifested, in people’s voices and in their facial expression, posture and basic muscle tone. If there’s exuberance coming from the upper part of a person’s face, and their voice has intonation modulation or what’s called prosody, we become attracted to the person. We like to talk to them – it’s part of our co-regulation.
So when we become polyvagal-informed, we start understanding not only the other person’s response but also our responsibility to smile and have inflection in our voice, to help the person we’re talking to help their body feel safe.”
Clink on the link below to hear Dr. Bessel van der Kolk, one of the world’s leading experts on developmental trauma, explain how our long-term health and happiness can be compromised by prior exposure to violence, emotional abuse, and other forms of traumatic stress.
Maybe you should Talk to SomeoneMaybe you should Talk to Someone
Author: Lori Gottlieb
Maybe you should talk to someone is a genuine, funny, touching, and realistic memoir of one therapist, as she navigates a difficult time in her professional and personal life. I couldn’t put this book down. As a therapeutic counsellor myself, the book gave me a greater understanding of psychology and human behaviour. It is a vulnerable portrayal of a renowned psychotherapist, her therapist, and the clients lives that she discusses in the book – and how they influence her life. If you have any preconceived bias about the therapy profession, this book might give you a new perspective. I laughed whole-heartedly and I blinked back the tears on one occasion. I’m really pleased I read Maybe You Should Talk About Someone. If you’re a busy person, the audio version may be more practical for you.