I want to preface this post by stating that the concepts and suggestions I’ve made below are my own thoughts, opinions, and suggestions based on my own experience working in the mental health sector and lived experience. There may also be numerous grammatical and logical errors. I know that you’re intuitive enough to understand what I’m attempting to describe and explain. Therefore, there will be no references section at the end. This is merely an expression of thoughts, a stream of consciousness (William James coined the term Stream of Consciousness).
Episodic, acute, and chronic anxiety can be miserable and debilitating. Individuals living with anxiety have generally experimented with many techniques to cope with anxiety symptoms, and they have often been practicing these techniques for months, years, or decades. Anxiety is life changing. Current treatment can be efficacious at reducing the intensity or frequency of symptoms for the vast majority of people living with anxiety, but only at best. I, myself, have tried the deep breathing technique commonly advised by mental health professionals, and it can be about as useful as taking a sugar pill. There is credible science that supports deep breathing exercises can improve symptoms and recovery rates for stress, anxiety and depression levels – but what about for an anxiety attack or a panic attack or intense chronic symptoms of anxiety?
Sometimes nothing is effective enough for immediate relief. It is my contention that building a relationship with a trained psychiatrist, specialised in this domain, is an essential first step. Your treating specialist(s) will need to have extensive experience and a comprehensive understanding of the debilitating impacts of anxiety, anxiety attacks, and/or panic attacks. I recommend psychiatry because you will need someone who can prescribe short-term medication, schedule 4 or greater, to alleviate the pain rapidly. All symptoms a person may experience from any condition in the anxiety family present a risk for searching for any immediate relief. This is true for you or me or anyone. Without prompt and effective medical care readily available, many people who do not have a plan for managing anxiety will potentially search for an unhealthy substitute to acquire relief.
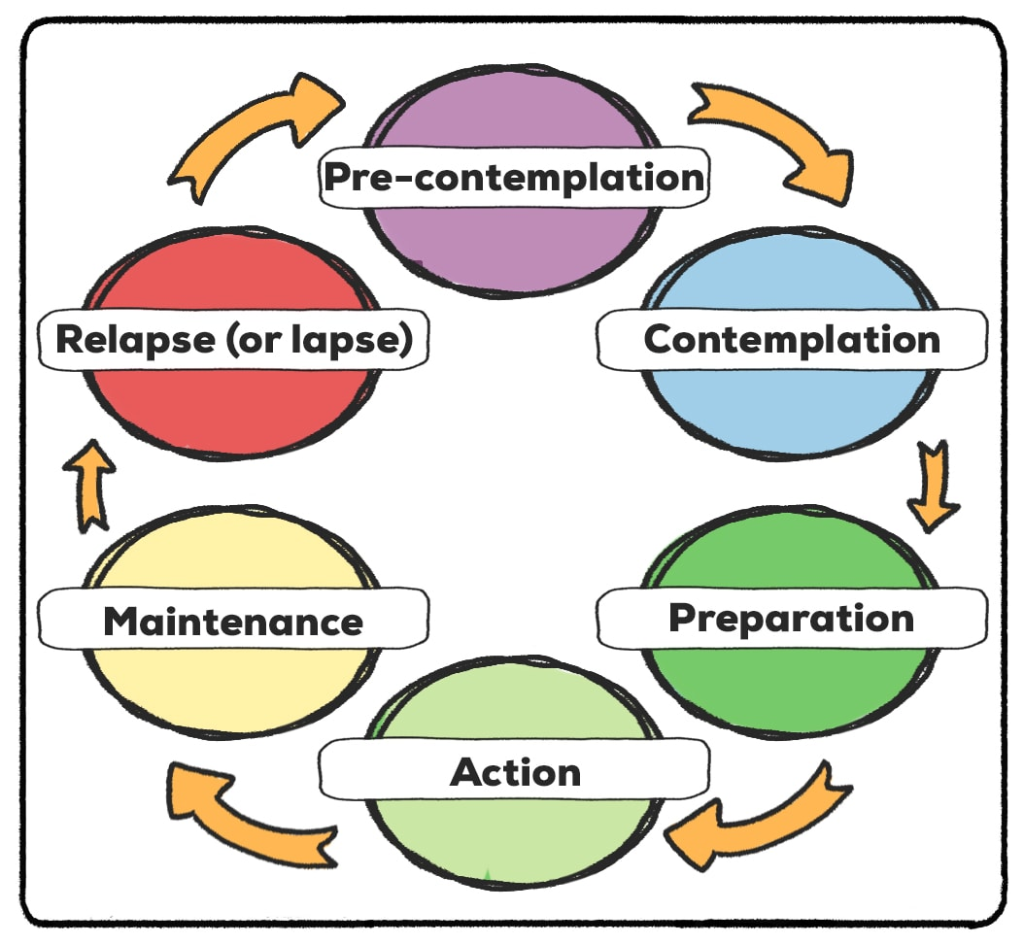
These substitutes are often unhelpful long term but effective short term. We all know what they are: alcohol and other drugs, sexual promiscuity or sex addiction, love addiction, gambling, excessive or unhealthy eating habits, self-injury, addictive forms of gaming, impulse spending, co-dependent or dependent behaviours on people, people pleasing, running away (avoiding reality), raging, reckless driving and other criminal behaviour, and relying on pharmaceuticals (legally prescribes or otherwise) that will have long-term unhealthy side effects. People know how to “doctor shop”, and although this area of medicine is becoming much more regulated, it still occurs. Unfortunately, there are people who do require certain types of legal drugs, in a timely manner, to find relief as a means of not engaging in any of the previously mentioned behaviours.
Some people may not have much faith in the field of psychiatry or psychology – HOWEVER – you may find yourself in a situation one day where you will need a doctor who knows your history to increase the likelihood of prescribing medication to treat anxiety when you need it most. This medication usually has addictive properties. An ethical psychiatrist will usually be unwilling to prescribe more than a single repeat of potentially addictive medication to treat their patients. This is standard, regulated medical practice in Australia.
Anyone working in the drug and alcohol sector or has regular contact with a person living with anxiety, or any form of addiction, will know that patients – people – are not being seen in a timely manner top treat anxiety before the patient starts looking elsewhere. Even once the patient has accessed some type of medical care, the length of care is not long enough for the patient to be “well enough” after discharge or ending their hourly session, to be on their own in the community safely without becoming vulnerable to their condition in a short time and looking for more relief to ease their pain and improve their well-being.
If a person or a patient cannot depend on the medical system in the way they need to feel safe and well, they will almost certainly begin to lose faith and trust in health professionals, and ‘the system’. This perpetuates their internalised stigma being reinforced, yet again.
I am not saying the patient doesn’t have a significant responsibly of their own to make valuable choices outside of medical treatment. I quote what someone once said to me, “You may not have asked for this disease, but it becomes our responsibility to stay well”. That is our duty as the person living with a health issue of any kind. There are things we certainly must do (or not do) to stay as healthy as possible. The help make not be there in a timely manner the next time we need immediate help.
It can take weeks or more to enter a detox facility. It can take months to enter a rehabilitation facility. It can take months for an available appointment to open with a psychiatrist. It becomes our responsibility to know that even when we’re feeling well and back to “normal”, we must continue those relationships with medication professionals. It becomes our responsibility to try alternative medicines if that’s something you’re interested in. Let’s face it, psychiatrists cease their practice, our professional relationship has reached it’s potential for adequate, loving care, or we want to try something new.
Start the process of finding a reliable, qualified, and credible psychiatrist today. I would recommend finding a counselling psychologist or other mental health professional that you have a productive and friendly working relationship with – and if you want to practice Buddhism, or acupuncture, or hypnotherapy, or any other complementary and alternative medicine – do it. If you want to connect with God – do it. If you want to see a naturopath – do it. Whatever it is, this may very well be a lifelong journey for you. Based on my own experience, don’t stop because you think you’re “all better now”. The previously mentioned professions or treatment options or lifestyle choices can be extremely expensive, but I would encourage you to save for it, find less expensive options. Sitting in church is free, or listening to an online guru can be the price or maintaining your mobile service bill.
I once knew of a fellow peer in treatment alongside me who said he saved money for years to travel overseas to have a procedure not available in Australia at the time for this purpose. He wanted blood transfusions and heat therapy for chronic pain that didn’t doctors could not determine had physiological origins. The peer was sure it had to, and medical investigations in Australia come up negative. The peer explained the theory behind blood transfusions and heat therapy – he believed – were supposed to improve his blood circulation and blood flow to treat the chronic pain he’d been living with for years after a workplace accident. Even this procedure overseas proved ineffective in mitigating his chronic pain. So, next he tried the wim hof method. He changed is diet. He exercised differently. He tried hypnotherapy. Finally, he turned psychology to treat stress and process childhood trauma. He was being treated for this a private facility where I was a patient at that time. I lost contact with him after I ended my own treatment episode. I don’t know if he’s still living with chronic pain or not.
The following are some very basic and well-known strategies in the Western world of psychology that you can begin to practice today, and then practice every day after that too – even for 5-20 minutes:
– learning about anxiety – your specific “causes” and the conditions more generally
– mindfulness
– relaxation techniques
– correct breathing techniques
– dietary adjustments
– exercise
– learning to be assertive
– building self-esteem
– cognitive therapy
– exposure therapy
– structured problem solving
– support groups
My firm believe is this:
Strong, healthy, quality relationships are essential to treating anxiety and other psychological illnesses. This about your life today: are you lonely (romantically or otherwise), are you a stressed individual, do you regularly feel like you job is stressful or unfulfilling, do you feel sad a lot, are you feeling pointless a lot, or feeling helpless a lot, feeling shame a lot, getting angry a lot over considerably minor things? etc. etc. etc. I would strongly encourage talking to a professional and begin exploring what options you have available to you.
Try, explore, play with a few methods of treatment. However, this must take a priority in your life. It must balance will all the many other obligations and responsibilities people encounter daily.
Type alternative medications or approaches to psychology. There are so many. It can be fun to try out a few when your finances permit. Even planning a holiday every 3-6 months is taking care of your well-being.
Many blessings friends.