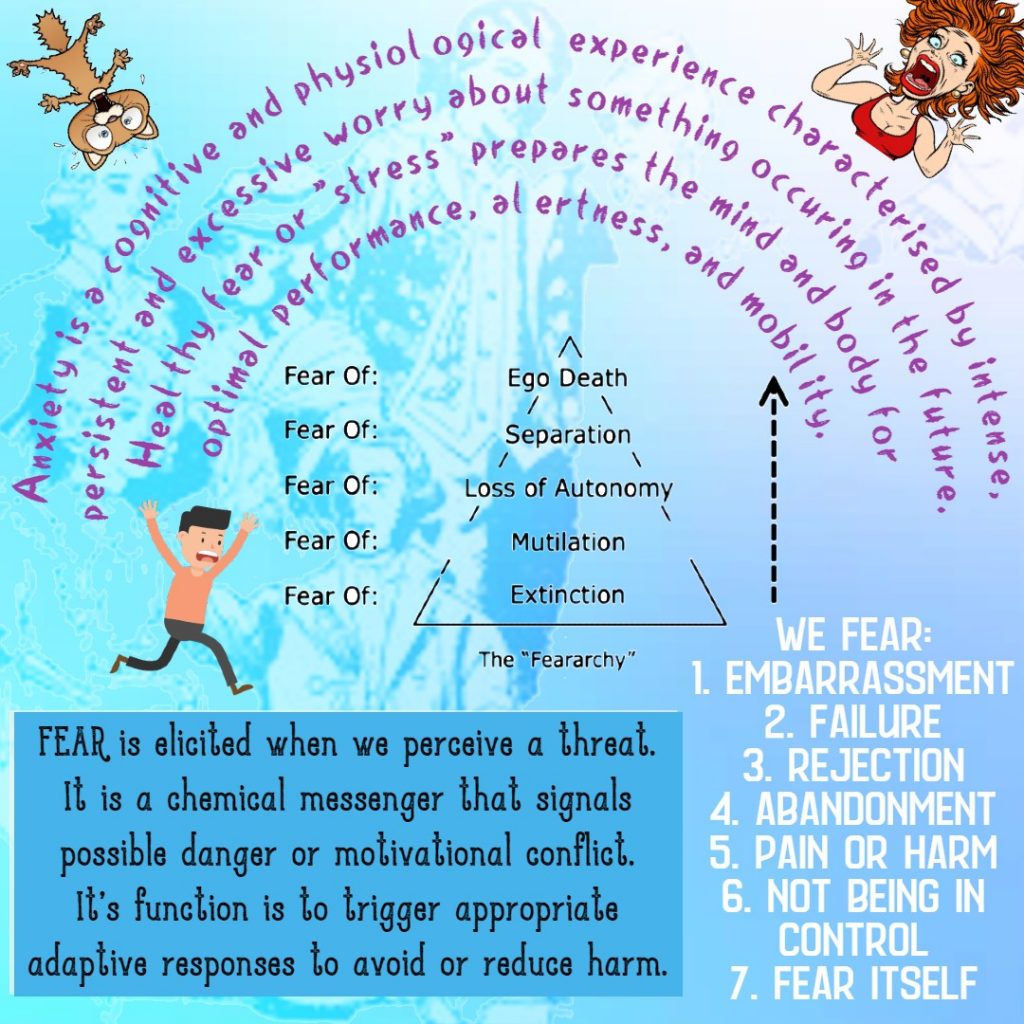
Shame is a complex and powerful (“contracting” and belittling) emotion that can have a significant impact on our mental health and how we navigate the world and interact with people. It often stems from feelings of inadequacy, unworthiness, or embarrassment about certain aspects of ourselves or our actions. This may not mean much to you right now … but that is all bullshit. I have worked with many people experiencing extreme toxic shame, and they are intrinsically beautiful people. Understanding the root causes of toxic shame is an essential first step in creating a healthy relationship with it. It’s crucial to recognize that experiencing shame is a universal human experience, and it does not define your worth as a person. Oftentimes, our shame is a projection of what we believe other people think about us, or it is an internalised belief (script, attitude etc.) that we learned from painful and scary life experiences. I want to preface the following by acknowledging that shame can be healthy. Without shame, we may develop unhealthy levels of egotism, narcissism, arrogance, and superiority.
The following are evidence-based, albeit typical, and clichéd approaches to building a healthy relationship with our toxic shame:
Challenge Negative Thoughts
One effective way to overcome shame is to challenge negative thoughts and beliefs that contribute to feelings of shame. This can feel exhausting! To be constantly vigilantly of our thinking, hence, noticing and letting thoughts stream through the mind will be necessary here. In 12-step fellowships, they would suggest to “let the go” and “hand them over”. For example, saying to yourself “This is not for me right now and I’ll hand it over to the universe just for now”. We do not always have the energy to challenge our negative thoughts. You can ‘compartmentalise them’, or say, “not right now”, or even say “thank you for making me aware of this and I may reflect on this when I have more time”. Challenging negative thoughts involves identifying and questioning the critical inner voice that fuels self-criticism and self-doubt. By practicing self-compassion and cultivating a more positive self-image, you can begin to counteract the destructive effects of shame. If you want someone to talk to about these issues, please call me: 0488 555 731.
Practice Self-Compassion
Self-compassion (and kindness) is a key component of overcoming shame. Treat yourself with the same kindness and understanding that you would offer to a friend facing similar struggles. Underpinning our shame is a profound fear that we will be rejected i.e., lose a job, be ignored by friends, lack confidence to make meaningful connections and intimacy. Acknowledge your imperfections without harsh judgment and remind yourself that it’s okay to be imperfect. We don’t often see others’ imperfections, and when we do, we think theirs are tolerable or not that bad compared to ours. Developing self-compassion can help us build resilience in the face of shame and cultivate a healthier relationship with yourself. I say again, every client I have worked with has shown me their absolute beautifulness by talking about their imperfections and showing me their self.
Seek Support
It’s essential to reach out for support when dealing with shame. This can be terrifying – paralysing even – and many people have reached out in the past and the outcome has made us feel even worse. Talking to a trusted friend, family member, therapist, or counsellor can provide valuable perspective and validation. Sharing your feelings of shame with others can help you feel less isolated and alone in your struggles. Additionally, professional help can offer guidance and strategies for coping with shame in a healthy way.
Cultivate Self-Acceptance
Practicing self-acceptance involves embracing all aspects of yourself, including those that may trigger feelings of shame. Recognize that nobody is perfect, and everyone makes mistakes. By accepting your vulnerabilities and imperfections, you can reduce the power that shame holds over you. Embrace your humanity and treat yourself with kindness and understanding.
Engage in Positive Activities
Engaging in activities that bring you joy, fulfillment, and a sense of accomplishment can help counteract feelings of shame. Pursue hobbies, interests, or goals that boost your self-esteem and remind you of your strengths and capabilities. Surround yourself with supportive people who uplift you and encourage your personal growth.
Practice Mindfulness
Mindfulness techniques can be beneficial in managing feelings of shame. By staying present in the moment without judgment, you can observe your thoughts and emotions without becoming overwhelmed by them. Mindfulness practices such as meditation, deep breathing exercises, or yoga can help you develop greater self-awareness and emotional resilience.
Top 3 Authoritative Sources Used:
- American Psychological Association (APA) – The APA provides evidence-based information on mental health issues, including strategies for coping with emotions like shame.
- Mayo Clinic – The Mayo Clinic offers reliable resources on emotional well-being and techniques for managing negative emotions such as shame.
- Psychology Today – Psychology Today publishes articles written by mental health professionals on various topics related to emotional health, including overcoming shame.
These strategies, actions, and ways of thinking will take practice, practice, and more practice. It is not easy. Based on my own experience, I needed a group of people on my path who I could rely on and practice with many times over, and then I started practising on my own. I still connect with the people living my recovery. I take breaks from them when I need to, but I always reconnect because loneliness will breed more shame. Please call 0488 555 731 if you need my support.