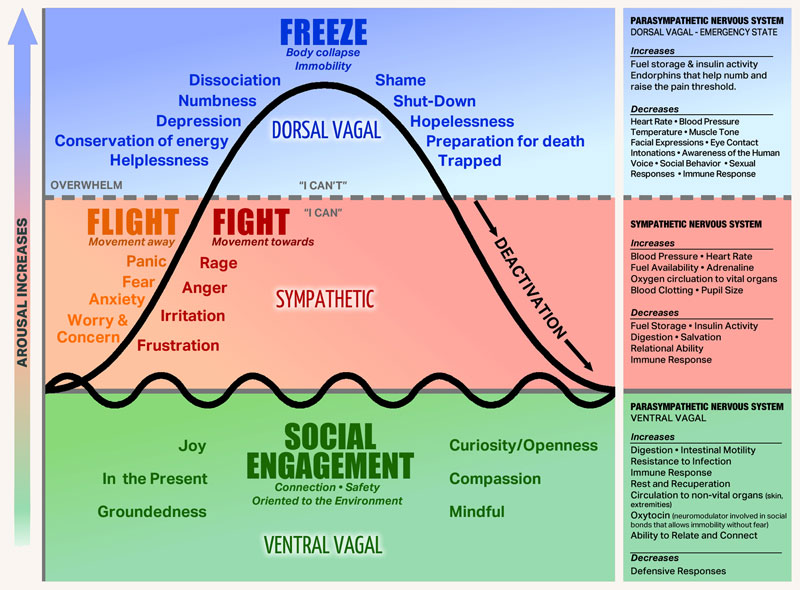
Stephen Porges, psychiatry professor and researcher, on the polyvagal theory he developed to understand our reactions to trauma:
[Paraphrased] Polyvagal theory articulates three branches of the autonomic nervous system (ANS) that evolved from primitive vertebrates to mammals. First, there is a system known as ‘freeze’, which involves death feigning or immobilisation. Second, the ANS has a ‘fight or flight’ system, which is a mobilisation system. And third, with mammals, there is what Porges calls, a social engagement system (SES), which can detect features of safety, and actually communicate them to another. The SES may also be referred to by some as ‘rest and digest’, which Porges theory suggests is a function of the Vagus Nerve – the tenth cranial nerve, a very long and wandering nerve that begins at the medulla oblongata. When an individual experiences feelings of safety (within an SES state), the autonomic nervous system can support health restoration. In terms of dealing with a life threat, an ordinary person will most likely go into a feigning death, dissociative state of ‘freeze’.
Polyvagal theory in psychotherapy offers emotional co-regulation as an interactive process between therapist and client which engages the social engagement system of both therapist and client. Social engagement provides experiences of safety, trust, mutuality and reciprocity in which we are open to receiving another person, just as they are.
The following extract has been retrived from https://www.theguardian.com/society/2019/jun/02/stephen-porges-interview-survivors-are-blamed-polyvagal-theory-fight-flight-psychiatry-ace
Polyvagal theory has made inroads into medical and psycho-therapeutic treatment, but how should it inform how people treat each other?
“When we become a polyvagal-informed society, we’re functionally capable of listening to and witnessing other people’s experiences, we don’t evaluate them. Listening is part of co-regulation: we become connected to others and this is what I call our biological imperative. So when you become polyvagal-informed you have a better understanding of your evolutionary heritage as a mammal. We become aware of how our physiological state is manifested, in people’s voices and in their facial expression, posture and basic muscle tone. If there’s exuberance coming from the upper part of a person’s face, and their voice has intonation modulation or what’s called prosody, we become attracted to the person. We like to talk to them – it’s part of our co-regulation.
So when we become polyvagal-informed, we start understanding not only the other person’s response but also our responsibility to smile and have inflection in our voice, to help the person we’re talking to help their body feel safe.”
Clink on the link below to hear Dr. Bessel van der Kolk, one of the world’s leading experts on developmental trauma, explain how our long-term health and happiness can be compromised by prior exposure to violence, emotional abuse, and other forms of traumatic stress.