Addiction is a chronic, relapsing disorder involving changes in brain reward, motivation, learning, stress and executive control systems. While different substances (and behaviours) act through distinct primary mechanisms, they converge on common neurobiological pathways — particularly the mesocorticolimbic dopamine system.
Below is an overview in Australian English of the core mechanisms and then substance-specific and behavioural addiction processes.
Core Neurobiological Pathways in Addiction
1. The Mesocorticolimbic Dopamine System
The central pathway implicated in addiction is the mesocorticolimbic circuit, involving:
- Ventral tegmental area (VTA)
- Nucleus accumbens (NAc)
- Prefrontal cortex (PFC)
- Amygdala
- Hippocampus
All addictive drugs increase dopamine transmission in the nucleus accumbens, either directly or indirectly. Dopamine does not simply produce pleasure — it encodes reward prediction, salience and learning. With repeated exposure:
- Drug-related cues gain exaggerated salience
- Natural rewards become less reinforcing
- Behaviour becomes increasingly habitual and compulsive
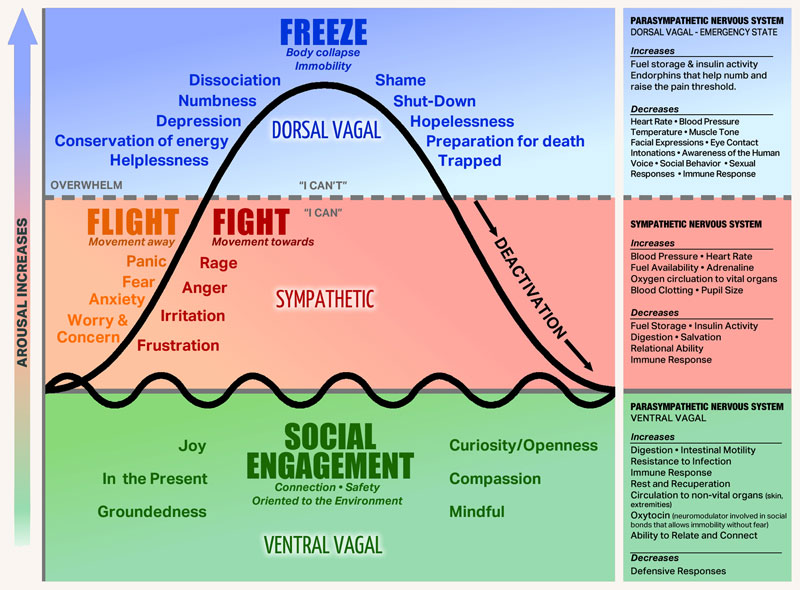
2. Neuroadaptation and Allostasis
Repeated substance exposure produces:
Tolerance — Reduced response due to receptor downregulation or neurotransmitter depletion.
Dependence — Neuroadaptations that produce withdrawal when the substance is removed.
Allostatic shift — The brain’s reward set point shifts downward, mediated by stress systems (e.g. corticotropin-releasing factor), resulting in dysphoria during abstinence.
3. Habit Formation and Loss of Control
With repeated use:
- Control shifts from ventral striatum (goal-directed) to dorsal striatum (habit-based)
- Prefrontal cortex regulation weakens
- Impulsivity and compulsivity increase
Substance-Specific Mechanisms
Alcohol
Alcohol acts on multiple neurotransmitter systems:
- Enhances GABA-A receptor function (inhibitory)
- Inhibits NMDA glutamate receptors (excitatory)
- Increases dopamine release in nucleus accumbens
- Affects endogenous opioid systems
Chronic exposure leads to:
- GABA downregulation
- NMDA upregulation
- Hyperexcitable state during withdrawal (risk of seizures, delirium tremens)
Alcohol dependence also involves stress system activation and impaired frontal cortical control.
Methamphetamine
Methamphetamine is a potent psychostimulant that:
- Enters presynaptic terminals
- Reverses the dopamine transporter (DAT), causing carrier-mediated dopamine efflux
- Inhibits vesicular monoamine transporter 2 (VMAT2), releasing dopamine from synaptic vesicles into the cytoplasm
- Causes massive dopamine release into the synapse
It also increases noradrenaline and serotonin.
Chronic use causes:
- Dopamine neurotoxicity (particularly to dopaminergic terminals)
- Reduced dopamine transporter availability
- Structural changes in striatum and PFC
- Persistent cognitive deficits
Methamphetamine produces particularly strong sensitisation of cue-driven craving.
Cocaine
Cocaine:
- Blocks the dopamine transporter (DAT), preventing reuptake
- Increases synaptic dopamine concentration
Unlike methamphetamine, cocaine acts by blocking DAT rather than reversing it, and does not cause large presynaptic vesicular release — the elevation in synaptic dopamine arises from impaired clearance.
Repeated use leads to:
- Dopamine receptor downregulation
- Enhanced cue reactivity
- Rapid cycling between intoxication and crash
- Strong psychological dependence
Opioids (e.g. heroin, morphine, oxycodone)
Opioids act primarily at mu-opioid receptors (MORs), which are expressed throughout the brain, including in the VTA. Their dopaminergic effects arise through multiple mechanisms:
- MORs on GABAergic interneurons in the VTA suppress inhibitory tone, thereby disinhibiting dopamine neurons (the classical disinhibition mechanism)
- MORs are also expressed on VTA dopamine neurons and projection targets directly, contributing additional excitatory drive beyond the disinhibition pathway
They also act in brainstem respiratory centres, which underlies the risk of respiratory depression in overdose.
Chronic use produces:
- Receptor desensitisation and internalisation
- Reduced endogenous opioid production
- Severe physical withdrawal mediated by noradrenergic rebound in the locus coeruleus
- Strong negative reinforcement (use to avoid withdrawal)
Cannabis
Δ9-tetrahydrocannabinol (THC):
- Activates CB1 receptors (the primary psychoactive cannabinoid receptor)
- Modulates GABA and glutamate release at presynaptic terminals
- Indirectly increases dopamine in NAc via disinhibitory mechanisms
Cannabis produces:
- Altered endocannabinoid system function
- CB1 receptor downregulation with chronic use
- A mild to moderate withdrawal syndrome (irritability, sleep disturbance, appetite changes)
- Effects on hippocampal memory circuits
While addiction risk is generally considered lower than for opioids or stimulants, it remains clinically significant and may be underestimated, particularly given the widespread availability of high-potency THC products (e.g. concentrates and high-THC flower), which are associated with greater dependence risk and more severe withdrawal.
MDMA (Ecstasy)
MDMA:
- Reverses the serotonin transporter (SERT), causing massive serotonin efflux — this is its primary mechanism
- Also increases dopamine and noradrenaline
Neurobiological consequences include:
- Acute empathogenic and entactogenic effects driven by serotonin release
- Post-use serotonin depletion, which may contribute to dysphoria in the days following use
- Potential serotonergic neurotoxicity, though this evidence comes largely from high-dose or repeated animal studies; the clinical significance in typical human recreational use remains under debate and is not definitively established
- Moderate addictive potential relative to psychostimulants, partly because dopaminergic effects are less prominent than with cocaine or methamphetamine
Prescription Psychoactive Medications
Certain prescribed medications also have addictive potential:
Benzodiazepines — Enhance GABA-A receptor activity. Cause tolerance via receptor downregulation. Dependence is primarily a GABAergic adaptation. Withdrawal can be protracted and, in cases of high-dose or long-term use, may produce seizures.
Prescription stimulants — Act via similar mechanisms to amphetamine, increasing dopamine and noradrenaline. Risk of misuse exists in susceptible individuals, though therapeutic doses in appropriately diagnosed patients are associated with substantially lower addiction risk than recreational use.
Behavioural (Process) Addictions
Gambling Disorder
Gambling disorder is recognised in DSM-5-TR as a non-substance-related addictive disorder. Although no substance is ingested, similar neurobiological mechanisms are involved.
Dopamine and reward prediction error — Near misses activate the nucleus accumbens similarly to wins. Variable ratio reinforcement schedules (as in poker machines) generate strong, unpredictable dopamine prediction error signalling that powerfully drives continued behaviour.
Cue reactivity — Gambling-related cues activate the same mesocorticolimbic circuitry as drug cues, with increased striatal activation and reduced prefrontal inhibitory control.
Habit circuitry — A shift from ventral to dorsal striatal control contributes to compulsive betting despite continued losses.
Other Emerging Behavioural Addictions
Conditions such as internet gaming disorder, compulsive sexual behaviour disorder, and problematic social media use share overlapping neurobiological features including:
- Dopamine dysregulation and sensitisation to cue salience
- Reduced executive control
- Stress system activation
However, the evidence base for most of these conditions is still developing, and their classification as formal addictive disorders remains an area of active research and debate. Internet gaming disorder is currently listed in DSM-5-TR as a condition for further study.
Shared Neurobiological Themes Across Addictions
Across substances and behaviours, addiction involves:
- Dopamine sensitisation to cues
- Reduced sensitivity to natural rewards
- Impaired prefrontal inhibitory control
- Stress system overactivation (particularly corticotropin-releasing factor)
- Habit circuitry dominance (dorsal striatum)
- Neuroplastic changes in glutamatergic signalling
Why Some Substances Are More Addictive
Addictive potential is influenced by multiple interacting factors. The speed of dopamine rise is one of the most studied — faster onset of dopamine elevation (e.g. via smoking or intravenous administration) is associated with stronger reinforcement. This framework, developed largely through the work of Volkow and colleagues, has strong empirical support, though it represents a mechanistic model rather than an established universal law. Other important factors include:
- Intensity of dopamine release
- Pharmacokinetics (e.g. route of administration)
- Withdrawal severity (which drives negative reinforcement)
- Social and environmental context
- Genetic vulnerability (heritability of addiction is estimated at 40–60% across substances)
Conclusion
Addiction is not simply about pleasure seeking. It reflects maladaptive neuroplasticity in reward, stress, learning and executive control circuits. While alcohol, methamphetamine, cannabis, opioids, cocaine and MDMA each act through different primary molecular mechanisms, they converge on common neural pathways that drive craving, tolerance, withdrawal and compulsive use. Behavioural addictions such as gambling engage these same circuits despite the absence of an ingested substance.
The neurobiological understanding of addiction continues to evolve, and where evidence is still emerging — particularly regarding emerging behavioural addictions and the long-term neurotoxic effects of substances like MDMA — clinical interpretation should be appropriately cautious.