Please click on the link for the article by BY ERIC LANGSHUR AND NATE KLEMP PHD
Two Science-backed Ways to Ease a Worried Mind.
Related Post
The continued differential treatment of mental illness and addiction compared to physical illness by broader society is rooted in several factors:The continued differential treatment of mental illness and addiction compared to physical illness by broader society is rooted in several factors:
Historical Context
Historically, mental illness and addiction have been misunderstood and stigmatized. For much of history, these conditions were seen as moral failings or character flaws rather than medical issues. This has led to a persistent stigma that continues to influence societal attitudes.
Lack of Awareness and Education
There is still a significant lack of awareness and education about mental health and addiction. Many people do not understand that these conditions are medical issues that require treatment, just like physical illnesses. This lack of understanding contributes to negative attitudes and discrimination.
Media Representation
Media often portrays mental illness and addiction in a negative light, reinforcing stereotypes and misconceptions. These portrayals can shape public perception and contribute to the stigma surrounding these conditions.
Criminalization
Addiction, in particular, has been heavily criminalised. This has led to a perception of addiction as a criminal issue rather than a health issue, further entrenching stigma and discrimination.
Internalised Stigma
Individuals with mental illness or addiction often internalise the stigma they experience, leading to feelings of shame and low self-worth. This can prevent them from seeking help and support, perpetuating the cycle of stigma and discrimination.
Healthcare System
Even within the healthcare system, biases and stigma can affect the quality of care provided to individuals with mental illness or addiction. This can lead to inadequate treatment and support, further exacerbating the issue.
Social and Cultural Factors
Social and cultural factors also play a role in how mental illness and addiction are perceived. Different cultures have varying attitudes towards these conditions, which can influence how they are treated and supported.
The differential treatment of treatment-resistant substance use disorder (SUD) and treatment-resistant cancer by society can be attributed to several factors:
1. Perception of Control
Substance use disorders are often perceived as a result of personal choices or moral failings, whereas cancer is seen as an uncontrollable disease. This perception leads to stigma and blame towards individuals with SUD, while those with cancer are more likely to receive sympathy and support.
2. Historical Stigma
Historically, substance use has been stigmatised and criminalised, leading to a societal view that addiction is a choice rather than a medical condition. In contrast, cancer has been recognized as a medical condition requiring treatment and compassion.
3. Media Representation
Media often portrays substance use in a negative light, emphasising criminality and moral failure. Cancer, on the other hand, is often depicted with empathy and urgency, highlighting the need for medical intervention and support.
4. Healthcare System
The healthcare system has historically been more equipped to handle cancer treatment, with extensive research, funding, and specialized care. SUD treatment has lagged behind, with fewer resources and less comprehensive care options.
5. Complexity of Treatment
Treatment-resistant SUD involves complex psychological, social, and biological factors, making it challenging to treat effectively. Cancer treatment resistance, while also complex, has seen significant advancements in research and technology, leading to more effective treatments.
6. Social and Cultural Factors
Cultural attitudes towards substance use and addiction vary widely, with some societies viewing it as a personal failing. Cancer is generally viewed more universally as a disease that requires medical intervention.
REFERENCES
Substance Use Disorder and Stigma
Australian Government Department of Health and Aged Care. (2024). Initiatives and programs. Retrieved from https://www.health.gov.au/about-us/what-we-do/initiatives-and-programs
Morrison, A. P., Birchwood, M., Pyle, M., Flach, C., Stewart, S. L. K., Byrne, R., Patterson, P., Jones, P. B., Fowler, D., & Gumley, A. I. (2013). Impact of cognitive therapy on internalised stigma in people with at-risk mental states. The British Journal of Psychiatry, 203(2), 140-145. https://doi.org/10.1192/bjp.bp.112.112110
Wood, L., Byrne, R., Burke, E., Enache, G., & Morrison, A. P. (2017). The impact of stigma on emotional distress and recovery from psychosis: The mediatory role of internalised shame and self-esteem. Retrieved from https://repository.essex.ac.uk/21927/1/woodpr2017.pdf
Cancer Treatment and Stigma
American Cancer Society. (2023). Cancer treatment and survivorship. Retrieved from https://www.cancer.org/treatment/treatments-and-side-effects.html
National Cancer Institute. (2022). Cancer treatment (PDQ)–Patient version. Retrieved from https://www.cancer.gov/types/treatment-pdq/patient/cancer-treatment-pdq
World Health Organization. (2021). Cancer treatment and palliative care. Retrieved from https://www.who.int/cancer/prevention/diagnosis-screening/cancer-treatment-palliative-care/en/
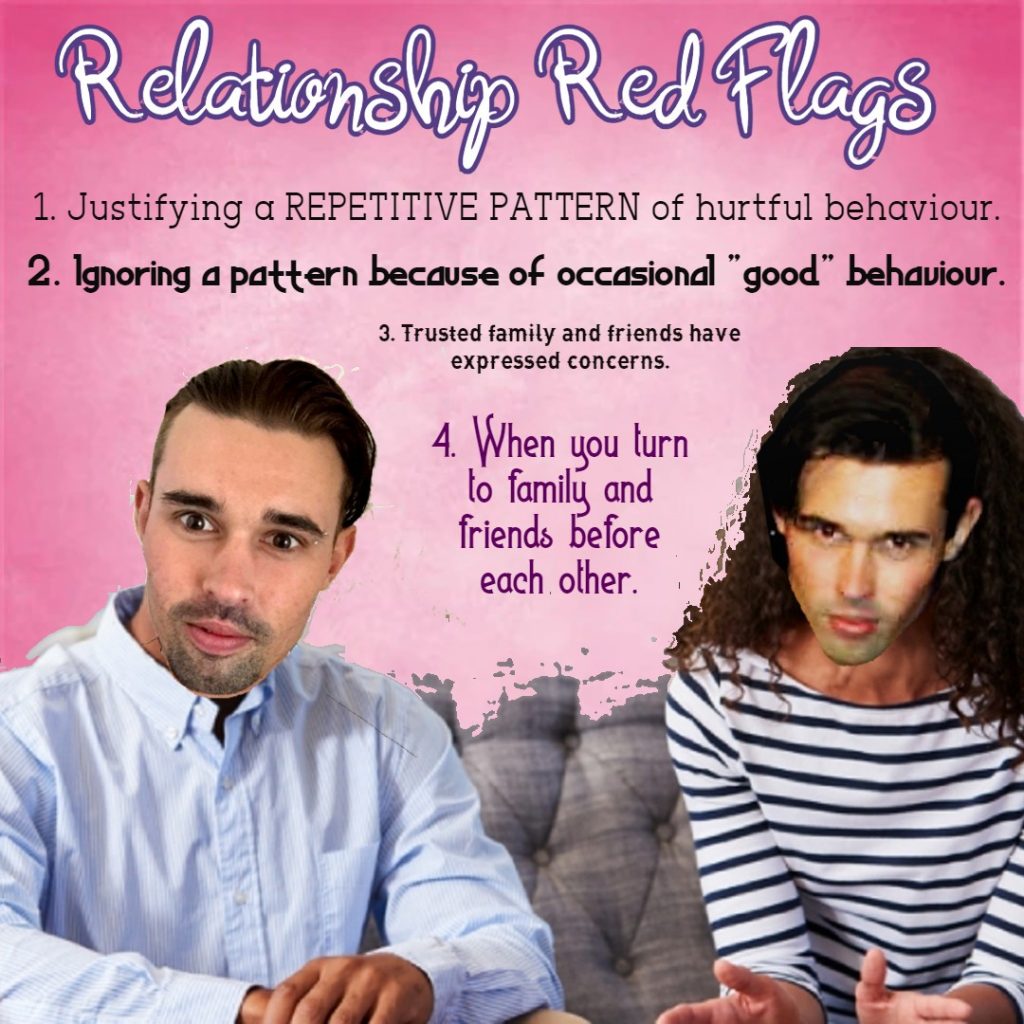
If we’re honest with ourselves, we know if a relationship isn’t working, if it is abusive or hurtful, or if it has run it’s course. We can ask trusted family and friends for their opinion if we’re confused or unsure.If we’re honest with ourselves, we know if a relationship isn’t working, if it is abusive or hurtful, or if it has run it’s course. We can ask trusted family and friends for their opinion if we’re confused or unsure.
Domestic Violence line (24 hours) 1800 65 64 63
Domestic violence services and support contact list | Family & Community Services (nsw.gov.au)
Emotions: Function and MotivationEmotions: Function and Motivation
Joy or happiness can motivate us to join in, take part, flourish, share, be a part of, repeat these activities.
Fear can motivate us to get away, hide, flee, run, keep ourselves or others safe. It protects us.
Sadness can motivate us to withdraw, ruminate, cry, heal, express hurt, seek comfort and bond with others.
Anger can motivate us to attack, defend or stand up for ourselves, identify boundary violation, identify there is a threat to our self or our loved ones or something we value.
Guilt can motivate us to repair what we have done and informs us that we have violated our morals or values.
Shame can motivate us to hide away, to keep things secret, to remember our fallibility and humility, to keep us “right sized”.
Disgust can motivate us to withdraw, keep a distance, get clean or clean our environment to ensure we stay healthy.
Compassion, empathy, or sympathy can motivate us to offer comfort, be with others, relate to one another and form strong bonds.
Confusion (Cognitive with physical sensations) can motivate us to get curious, learn, discover, grow.
Affection (behavioural with physical sensations) can motivate us to give love, get close to specific people who were feel safe with, and want to spend more time with.
