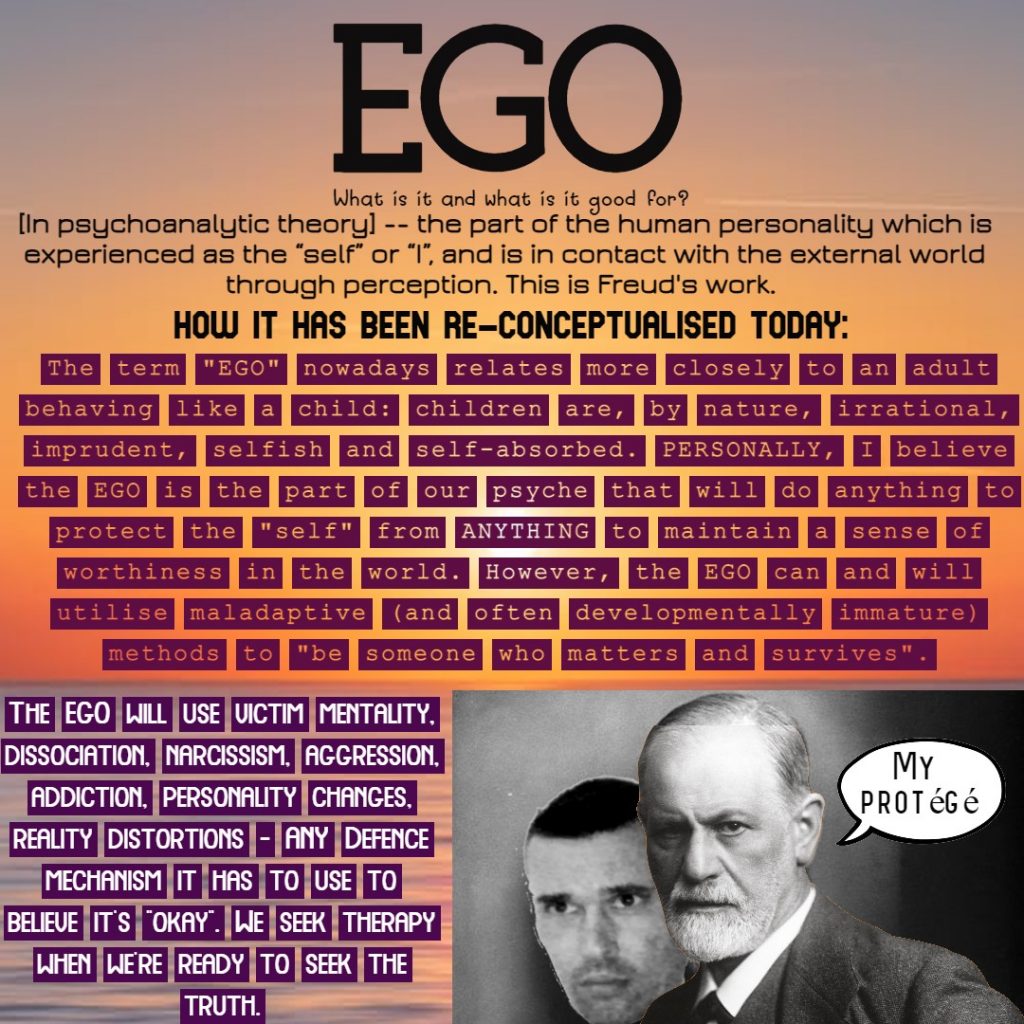
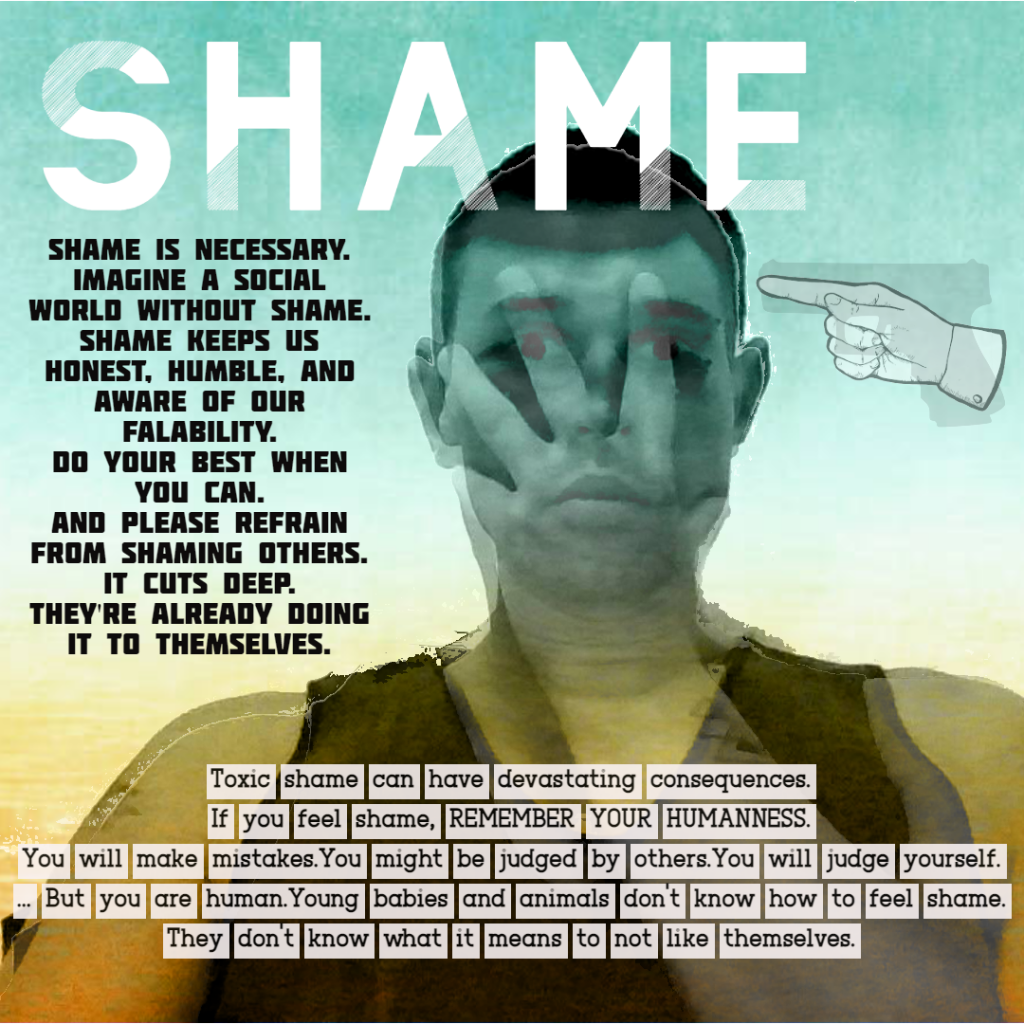
Despite significant advancements in political and health initiatives by governments and non-governmental organisations, shame, stigma, and internalized stigma continue to profoundly impact millions of lives worldwide. These negative perceptions and self-judgments can lead to feelings of worthlessness, self-blame, and social withdrawal, which in turn hinder access to services and participation in treatment.
Shame and stigma are particularly prevalent among individuals with substance use disorders, mental health conditions, and those experiencing psychosis. For instance, internalised stigma can lead to low self-esteem, depression, and hopelessness, which significantly impede recovery and emotional well-being. Even with the implementation of cognitive therapy and other supportive measures, the battle against internalised stigma remains ongoing in a similar fashion to intergenerational trauma, as though it has been built into human DNA.
Political and health initiatives have attempted to be instrumental in addressing these issues. For example, the Australian Government Department of Health and Aged Care has launched numerous programs aimed at improving health outcomes and reducing stigma. These initiatives focus on health promotion, early intervention, and disease prevention, aiming to create supportive environments for those affected by stigma.
However, the persistence of shame and stigma highlights the need for continued efforts to combat these issues especially in the workplace and within individual families. Addressing stigma therapeutically, promoting empathy and non-judgmental attitudes, and supporting individuals to view themselves beyond their conditions are crucial steps in mitigating the negative impacts of stigma.
Helping someone with a substance use disorder (SUD) while protecting yourself and your family involves a delicate balance of support and self-care. Here are some steps you can take:
1. Educate Yourself
Understanding SUD and its effects can help you make informed decisions and provide better support. Reliable sources include medical professionals, reputable websites, and support groups.
2. Set Boundaries
Establish clear boundaries to protect your well-being. This might include rules about substance use in the home, financial support, and personal interactions. Boundaries help prevent enabling behaviours and reduce stress.
3. Practice Self-Care
Taking care of yourself is crucial. Engage in activities that bring you joy and relaxation, such as exercise, hobbies, or spending time with friends. Self-care helps you maintain your mental and emotional health.
4. Seek Support
Join support groups like Al-Anon or seek therapy to process your emotions and develop coping strategies. Connecting with others who are going through similar experiences can provide invaluable support and understanding.
5. Encourage Professional Help
Encourage your loved one to seek professional help, such as counselling, therapy, or medical treatment. Treatment programs often include individual, group, or family therapy sessions, which can be beneficial for everyone involved.
6. Detach with Love
Detaching with love means setting emotional and psychological boundaries while still offering support. This approach helps you avoid becoming emotionally drained and allows your loved one to face the consequences of their actions.
7. Be Patient and Compassionate
Recovery is a journey that takes time. Be patient and compassionate with your loved one and yourself. Celebrate small victories and stay hopeful.
8. Avoid Judgment
Avoid being judgmental when discussing substance use. Offer support and understanding instead of criticism, which can help reduce feelings of shame and stigma.
References
Al-Anon Family Groups. (n.d.). Al-Anon and Alateen. Retrieved from https://al-anon.org/newcomers/what-is-al-anon-and-alateen
Australian Government Department of Health and Aged Care. (2024). Initiatives and programs. Retrieved from https://www.health.gov.au/about-us/what-we-do/initiatives-and-programs
Australian Institute of Health and Welfare. (2024). Health promotion and health protection. Retrieved from https://www.aihw.gov.au/reports/australias-health/health-promotion
Australian Government Department of Health. (2019). Alcohol and other drugs – Information for families. Retrieved from https://www.health.gov.au/resources/collections/alcohol-and-other-drugs-information-for-families
Mental Health Foundation. (2016). How to cope when supporting someone else. Retrieved from https://www.mentalhealth.org.uk/publications/how-cope-when-supporting-someone-else
Morrison, A. P., Birchwood, M., Pyle, M., Flach, C., Stewart, S. L. K., Byrne, R., Patterson, P., Jones, P. B., Fowler, D., & Gumley, A. I. (2013). Impact of cognitive therapy on internalised stigma in people with at-risk mental states. The British Journal of Psychiatry, 203(2), 140-145. https://doi.org/10.1192/bjp.bp.112.112110
National Institute on Drug Abuse. (2020). Family support in addiction recovery. Retrieved from https://www.drugabuse.gov/publications/principles-adolescent-substance-use-disorder-treatment-research-based-guide/family-support-in-addiction-recovery
Substance Abuse and Mental Health Services Administration. (2015). Substance use disorders. Retrieved from https://www.samhsa.gov/find-help/disorders
Wood, L., Byrne, R., Burke, E., Enache, G., & Morrison, A. P. (2017). The impact of stigma on emotional distress and recovery from psychosis: The mediatory role of internalised shame and self-esteem. Retrieved from https://repository.essex.ac.uk/21927/1/woodpr2017.pdf
Your Room. (2021). Shame and self-stigma. Retrieved from https://yourroom.health.nsw.gov.au/whats-new/Pages/Shame-and-self-stigma.aspx