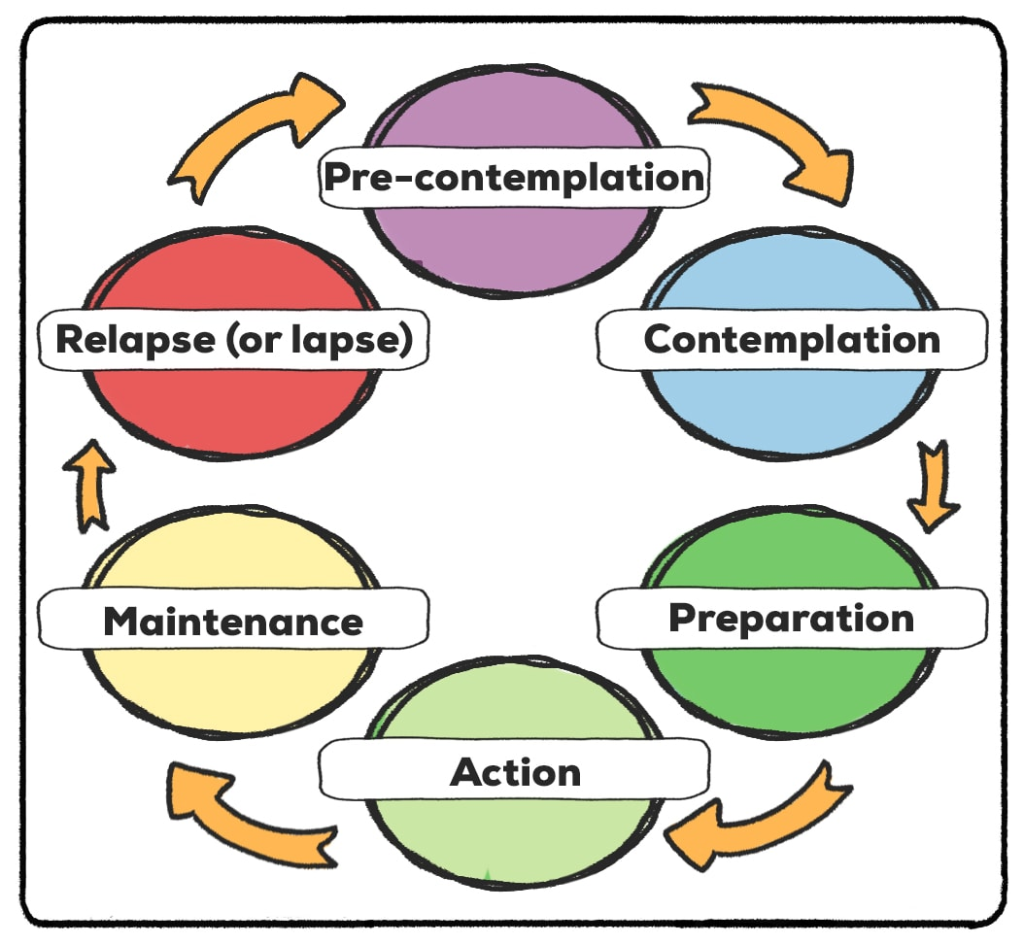
‘The stages of change model’ was developed by Prochaska and DiClemente. Heard of them? It informs the development of brief and ongoing intervention strategies by providing a framework for what interventions/strategies are useful for particular individuals. Practitioners need an understanding of which ‘stage of change’ a person is in so that the most appropriate strategy for the individual client is selected.
There are five common stages within the Stages of Change model and a 6th known as “relapse”:
1. In the precontemplation stage, the person is either unaware of a problem that needs to be addressed OR aware of it but unwilling to change the problematic behaviour [or a behaviour they want to change. It does not always have to be labelled as “problematic”].
2. This is followed by a contemplation stage, characterized by ambivalence regarding the problem behaviour and in which the advantages and disadvantages of the behaviour, and of changing it, are evaluated, leading in many cases to decision-making.
3. In the preparation stage, a resolution to change is made, accompanied by a commitment to a plan of action. It is not uncommon for an individual to return to the contemplation stage or stay in the preparation stage for a while, for many reasons.
4. This plan is executed in the action stage, in which the individual engages in activities designed to bring change about and in coping with difficulties that arise.
5. If successful action is sustained, the person moves to the maintenance stage, in which an effort is made to consolidate the changes that have been made. Once these changes have been integrated into the lifestyle, the individual exits from the stages of change.
6. Relapse, however, is common, and it may take several journeys around the cycle of change, known as “recycling”, before change becomes permanent i.e., a lifestyle change; a sustainable change.
(Adapted from Heather & Honekopp, 2017)